Return to Bioenergetic Support Page
Carnitine in Heart Attack
Co-Q10 is of value in heart attack, both as an antioxidant, and for its key role in energy metabolism. So far, in every condition where CoQ10 is of value, its partner in energy metabolism, carnitine, has also been shown to be helpful. This section reviews several studies demonstrating benefits of carnitine in acute heart attack.
Open Study of Carnitine and Post-MI Status and Mortality
Carnitine and Infarct Expansion
Carnitine and Acute Arrhythmia
Randomized, Double Blind Study of Carnitine and Post-Heart Attack Metabolic Status and Outcome
Heart attack is associated with a marked, sudden reduction in oxygen supply to the affected heart muscle. Without oxygen, fatty acids cannot be burned to generate ATP. Fatty acid levels will rise within the heart cells, where they can produce toxicity, but early on the fatty acids can be bound up and sequestered (buffered) by free carnitine, but this takes free carnitine out of action, compromising an already disordered state of energy production. Eventually the carnitine buffering capacity is overwhelmed; free fatty acids leave the affected cell and damage adjacent cells. Without carnitine, the oxygen starved cells cannot make use of the little oxygen still available to them. Anaerobic (oxygen independent) metabolism kicks in, generating metabolic acids. Energy failure ensues. The cell cannot make ATP. The cell membrane ruptures and the cell dies.
Oral carnitine takes a little while to get in to cardiac cells, while IV carnitine enters readily. Flooding the oxygen starved, energy deficient, acidotic, fatty acid rich myocardial cells with carnitine will buffer the fatty acid level, re-route the fatty acids into energy metabolism, and increase the supply of ATP available. If more ATP is available, cell function will improve, and the cell is less likely to die. The fewer heart cells that die, the less likely you are to die from a heart attack. Carnitine should limit the amount of damage sustained in a heart attack, and it should improve one's outcome following a heart attack. Let's look at the studies:
Open Study of Carnitine and Post-MI Status and Mortality
160 consecutive heart attack survivors were randomized to receive either placebo or carnitine at a dose of 4,000 mg/day. At 12 months, the carnitine supplemented patients had lower heart rate, blood pressure, and cholesterol values. Angina and arrhythmia were less frequent. 12.5% of the placebo treated post-heart attack patients had died, primarily from heart failure or recurrent heart attack. Only one of the 80 carnitine treated patients had died. This study was not double blind; the subjects and the researchers knew who was and who was not taking carnitine. Still, the results are impressive, and this study lead to several others, aiming to corroborate the carnitine benefit and to try to understand just how carnitine improved outcome in the post-heart attack setting.
Carnitine and Infarct Expansion
Infarct expansion, eventually to produce a cardiac wall aneurysm, portends a poor prognosis following a heart attack. Most heart attacks are incomplete. Not all the cells in the distribution of the blocked artery die, and some residual contractile function of the affected cardiac wall will remain. In a large or full thickness heart attack, no residual function remains. The heart muscle supplied by the still patent arteries, whipped into hyperdrive by adrenalin, will pump vigorously, while the dead cardiac segments will bulge out. The dead area will expand, disturbing the mechanics of contraction elsewhere. Heart performance will fall off, an aneurysm can form, and CHF ensues. Any therapy that limits heart attack size or attenuates cell death in the cardiac regions involved in the heart attack might decrease infarct expansion and prevent the overall increase in post-heart attack cardiac chamber size that we really do not want to see.
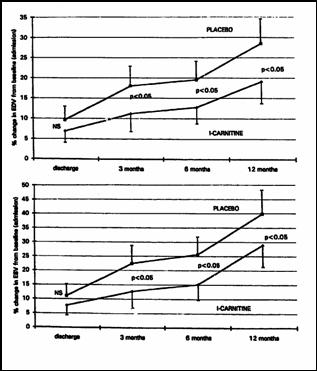
In this study 472 consecutive patients presenting with a heart attack involving the anterior wall of the heart were randomized to receive carnitine 6,000 mg/day or placebo over their first year post-heart attack. An echo study was carried out at hospital discharge and then periodically thereafter.
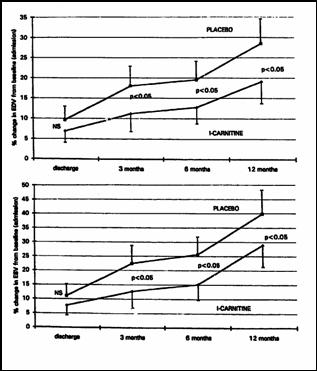
The top graph describes end-diastolic volume (in between beats) and the bottom graph describes end-systolic (as the heart is beating) volume of the heart. The upper line in both graphs is the placebo group and beneath it is the carnitine group. You can see that the heart enlarges post-heart attack in both groups, but that it is smaller at hospital discharge in the carnitine group (heart muscle was spared) and that it doesn't enlarge as much over the first year post-heart attack with carnitine on board. The mechanics of cardiac contraction will be thus less stressed. The heart segments not lost in the original heart attack will not be forced to make as much extra ATP, and they will be less likely to experience bioenergetic failure themselves.
Carnitine and Acute Arrhythmia
56 patients presenting with heart attack were randomized to receive IV placebo or IV carnitine at a dose of 100 mg/kg twice a day over three days, with continuous monitoring of cardiac rhythm:.
All measures of cardiac arrhythmia were less in the carnitine treated patients. Carnitine administration blunts acidosis, a condition that may initiate or aggravate arrhythmia, and by preserving energy metabolism oxidative stress in blunted, and thus another whip is sheathed. Smaller heart attacks are associated with a lower tendency to arrhythmia, and carnitine certainly limits the damage done following an interruption in oxygen supply to the heart.
Randomized, Double Blind Study of Carnitine and Post-Heart Attack Metabolic Status and Outcome
101 consecutive patients presenting with suspected heart attack
were randomized to receive carnitine 2,000 mg/day or placebo over 28 days, along
with standard medical therapy. First let's look at markers of free radical
stress and infarct size: 
 .
.
Less disorder in energy metabolism leads to lowered oxidative stress so lipid peroxide levels (a marker of oxidative stress) will fall with carnitine supplementation. The release of CK reflects the extent of damage, as does the EKG QRS score; it appears that carnitine administration spared heart muscle. Thus we would expect to see lower complication rates over the 28 day treatment period:
No surprises here. Heart muscle was spared, energy production was enhanced, there was less oxidative stress and acidosis, so as expected, outcome was improved. CoQ10, antioxidants, mineral supplementation (potassium and magnesium), fish oils, and antioxidant vitamins have all been shown to improve outcome, above and beyond standard drug therapy, in acute heart attack.
James C. Roberts MD FACC
1/01/07