Return to Bioenergetic Support Page
Ribose in Energy Metabolism
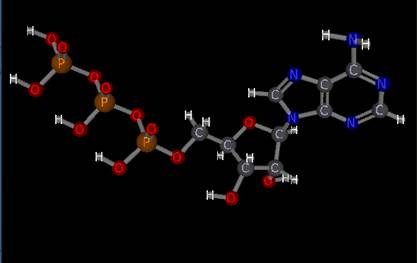
ATP, adenosine triphosphate, is the only energy source that our body can utilize to carry out biochemical reactions. Man's struggle for survival is really man's struggle, not to generate ATP, but rather to regenerate ATP. At least that was Mother Nature's plan.
ATP is precious stuff, and the heart, which never rests, needs a lot of it. Mother Nature did not construct the heart like a camel, with the ability to store a great deal of ATP. Rather, she endowed us with a great capacity to regenerate ATP. The average person possesses 700 mg of ATP in their heart. That might sound like a lot, but at a heart rate of 60 we will burn 70 mg of ATP every second; thus our entire 700 mg supply of ATP will last 10 heartbeats, around 10 seconds. The heart beats about 86,000 times each day, using up 6 million molecules of ATP, so each molecule of ATP in the heart must be regenerated 10,000 times each day. If not we die. Mother Nature believes in just in time ATP production. The basic plan is as follows:

The energy stored in the carbon-electron bond in the food that we consume is converted into a "high energy" bond, between ADP and phosphate to make ATP. As long as we have oxygen, food, and co-factors such as CoQ10 and carnitine, we can regenerate each ATP molecule as often as we need to. When we exercise, we need more ATP. We thus burn more sugar and fat, in the presence of oxygen (this process is called oxidative phosphorylation), and regenerate ATP from ADP. It is critical that we upregulate ATP regeneration to keep up with ATP expenditure, as if the concentration of ATP within the cell dips, critical cellular functions will falter. ATP isn't just a metabolic fuel, it is also the promoter and regulator of our biochemistry. A high level of ATP is the driving force behind all useful chemical reactions in the body. A high level of ATP pushes chemical reactions "to the right", in the direction of completion. When cardiac ATP levels fall, the last thing to go is cardiac contractile function. Well before this happens, cellular repair and metabolic function become compromised; protein biosynthesis falters, and the concentration of electrolytes across the cell membrane is affected adversely. The graphic below tells the story:
So if we run low on oxygen, as occurs in coronary artery disease, or if oxygen supply is temporarily shut off, as occurs in open heart surgery, or if ATP demand outstrips supply, such as when a healthy person sprints 200 yards or runs a Marathon, or in the cardiomyopathy patient's heart where CoQ10 and carnitine deficiency preclude normal ATP regeneration, then what happens?
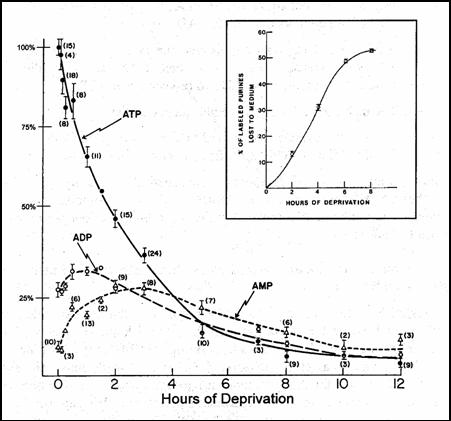
Without oxygen, we cannot regenerate ATP from ADP. We do have the ability to burn sugar in the absence of oxygen (anaerobic glycolysis, but this process is inefficient and cannot sustain life for very long - how long can you hold your breath under water?). There is still energy present within ADP, in the high energy bond between AMP and phosphorus. However, we cannot use ADP to carry out biochemical work; our enzyme systems only recognize ATP. So Mother Nature gave us an emergency back up system - we can combine two molecules of ADP to make one ATP and one AMP. We burn thought this ATP in a few seconds. Then we split phosphorus from AMP to form adenosine. Now, ATP, ADP, and AMP are all charged particles; as such they cannot diffuse across the cell membrane. Adenosine is not charged, so any adenosine generated as a consequence of energy failure is free to leave the cell, never to return. The graphic below shows what happens to intracellular ATP, ADP, and AMP levels when the heart muscle is deprived of oxygen. The inset shows the percentage of the total adenine nucleotide pool that is irreversibly lost - basically the longer the period of oxygen deficiency, the greater will be the irreversible loss of adenosine.
 At this point, the cell is facing death; it is out of ATP
energy, with no prospects to generate more. The cell will die, that is,
unless we decide to stop walking. If we stop walking when we are
experiencing angina, which is occurring only because we have run out of ATP,
blood supply will have a chance to catch up with demand and our ATP levels will
rise back to normal - well not all the way back to normal. You see, during
the period of time that the heart muscle cell was trying to function in a low
oxygen environment, a certain percentage of its adenine nucleotide pool (ATP +
ADP + AMP) was burned down to adenosine and lost forever. Even though our
oxygen supply has been restored, even thought we can participate in oxidative
phosphorylation, burning sugar and fat in an efficient, oxygen utilizing
fashion, we cannot return the intracellular ATP concentration to its prior
level. We can't refill our ATP tank because we have lost a percentage of
our adenine nucleotide pool, the building blocks of ATP regeneration. The
percentage lost will be a function of how long and to what degree that the heart
muscle was deprived of oxygen. If oxygen deficiency was brief, little
adenosine will be lost, but if we are experiencing angina throughout the day,
then adenosine deficiency will be pronounced. If an artery closes and we
begin to experience a heart attack, adenosine loss will be severe.
At this point, the cell is facing death; it is out of ATP
energy, with no prospects to generate more. The cell will die, that is,
unless we decide to stop walking. If we stop walking when we are
experiencing angina, which is occurring only because we have run out of ATP,
blood supply will have a chance to catch up with demand and our ATP levels will
rise back to normal - well not all the way back to normal. You see, during
the period of time that the heart muscle cell was trying to function in a low
oxygen environment, a certain percentage of its adenine nucleotide pool (ATP +
ADP + AMP) was burned down to adenosine and lost forever. Even though our
oxygen supply has been restored, even thought we can participate in oxidative
phosphorylation, burning sugar and fat in an efficient, oxygen utilizing
fashion, we cannot return the intracellular ATP concentration to its prior
level. We can't refill our ATP tank because we have lost a percentage of
our adenine nucleotide pool, the building blocks of ATP regeneration. The
percentage lost will be a function of how long and to what degree that the heart
muscle was deprived of oxygen. If oxygen deficiency was brief, little
adenosine will be lost, but if we are experiencing angina throughout the day,
then adenosine deficiency will be pronounced. If an artery closes and we
begin to experience a heart attack, adenosine loss will be severe.
 But
what if we carry out an emergency angioplasty or bypass surgery, restoring blood
supply and salvaging heart muscle? The muscle may be ultimately salvaged,
but it will not regain function until its adenine nucleotide pool has been
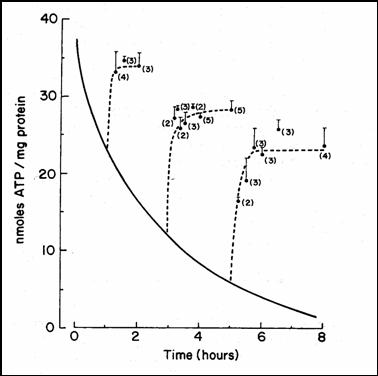
regenerated. The graphic to the left describes loss of intracellular ATP
as a function of duration of oxygen deficiency. The broken lines describe
the time course and degree of ATP regeneration if oxygen is suddenly resupplied.
As you can see, the longer the duration of oxygen deficiency, the lower will be
your new ATP concentration. Following open heart surgery or during your
recovery from a heart attack, you will left with a low ATP level. Your
heart muscle may be alive, but it will not function well, because it cannot make
adequate ATP, because it lost too much adenosine. The salvaged but ATP
deficient heart will be "stunned". If you are experiencing angina several
times a day, you too will suffer from adenosine burn off. Your heart will
be ATP deficient, and it will be stiff. This is why you experience
shortness of breath with effort, even when you are not experiencing angina -
your heart is now stiff because it cannot make enough ATP to relax properly.
Why do you feel poorly for several days after your stress test? I pushed
you on the treadmill, but now you are sitting at home, watching TV, and you may
still not feel right. You don't feel back to normal as during the stress
EKG I pushed you to the point of ischemia, relative oxygen deficiency within the
heart muscle. Some of your ATP was burned down to adenosine, which was
lost, and until you can regenerate adenosine (actually, it is AMP that needs to
be regenerated), you will not be able to return your ATP content back to
baseline. So how does our body regenerate AMP?
But
what if we carry out an emergency angioplasty or bypass surgery, restoring blood
supply and salvaging heart muscle? The muscle may be ultimately salvaged,
but it will not regain function until its adenine nucleotide pool has been
regenerated. The graphic to the left describes loss of intracellular ATP
as a function of duration of oxygen deficiency. The broken lines describe
the time course and degree of ATP regeneration if oxygen is suddenly resupplied.
As you can see, the longer the duration of oxygen deficiency, the lower will be
your new ATP concentration. Following open heart surgery or during your
recovery from a heart attack, you will left with a low ATP level. Your
heart muscle may be alive, but it will not function well, because it cannot make
adequate ATP, because it lost too much adenosine. The salvaged but ATP
deficient heart will be "stunned". If you are experiencing angina several
times a day, you too will suffer from adenosine burn off. Your heart will
be ATP deficient, and it will be stiff. This is why you experience
shortness of breath with effort, even when you are not experiencing angina -
your heart is now stiff because it cannot make enough ATP to relax properly.
Why do you feel poorly for several days after your stress test? I pushed
you on the treadmill, but now you are sitting at home, watching TV, and you may
still not feel right. You don't feel back to normal as during the stress
EKG I pushed you to the point of ischemia, relative oxygen deficiency within the
heart muscle. Some of your ATP was burned down to adenosine, which was
lost, and until you can regenerate adenosine (actually, it is AMP that needs to
be regenerated), you will not be able to return your ATP content back to
baseline. So how does our body regenerate AMP?
 This
is a problem.
This
is a problem.
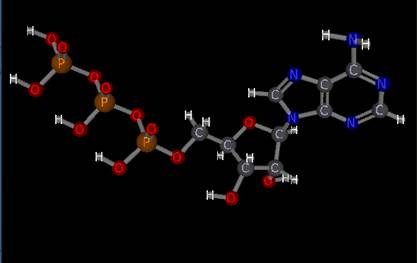
Mother Nature did not design us to synthesize AMP, at least not at a high level. She didn't anticipate that we would have coronary disease, that we would need to rapidly reconstitute our AMP supply. The rate limiting step in "from scratch" AMP synthesis is the generation of ribose, a five carbon sugar, from dietary glucose, a six carbon sugar. To make AMP from scratch, via the ribose biosynthetic pathway, takes weeks, and a lot of ATP energy. If you are recovering from bypass surgery or if you have just sustained a heart attack, you don't really have weeks, and you certainly don't have any ATP energy to spare to make ribose. This is a bad situation. The biosynthesis of new AMP, necessary to allow the heart to "unstun", is slow and metabolically expensive.
However, Mother Nature did give us a break. There is a "salvage pathway", whereby adenosine and its breakdown products (adenine and hypoxanthine) can be rapidly converted back in to AMP. If ribose is present in the cell in high concentration, the adenosine that is produced as a consequence of energy failure can be rapidly recycled back in to AMP, giving the cell the building block it needs to regenerate ATP. If we can get ribose in to the recently or chronically oxygen starved cell, we can accelerate the energetic recovery from oxygen deficiency; we can rapidly "unstun" the heart. As it turns out, supplemental ribose enters the cardiac cells rapidly, following either IV or oral administration. This is the basis for ribose supplementation in coronary disease, CHF, and for athletes. Studies demonstrating the benefits of ribose in these situations are presented elsewhere in the bioenergetic support section of this website. The study below describes the effect of ribose supplementation in an animal model of heart attack:
In this study, dogs were placed on cardiopulmonary bypass, and their hearts were deprived of oxygen for twenty minutes. Twenty minutes of oxygen deprivation is not long enough to kill the cardiac cells of a dog, but it is long enough to burn much of their ATP down to adenosine, such that following "reperfusion", the heart will be severely ATP deficient, and will stay that way until new ribose and new AMP can be generated from scratch. The graphics below describe left ventricular compliance (the elasticity or ability of the heart to fill, which is energy dependent) along with the ATP content of the recently oxygen deprived heart. You can see that these values fall and then recover in tandem, because left ventricular compliance is energy dependent. The heart will be stiff and ATP deficient for a full week following oxygen deficiency, because not enough time has elapsed for this stunned heart to synthesize enough ribose and AMP to allow reconstitution of its ATP supply..
But what would happen if we supplied this recently oxygen deprived, AMP deficient heart with ribose?
Here we look at ATP regeneration in the hearts of oxygen deprived dogs who received IV ribose or IV saline during their recovery from oxygen deficiency. The ribose treated animals resumed ATP production within four hours. The supplemental ribose they received was used to convert adenosine back in to AMP. So now that they have oxygen, they can burn sugar and fat and do something useful with this caloric energy - they can use it to convert AMP to ADP and then on to ATP. The non-supplemented dogs have no AMP, so they cannot make ATP, even though they now have a normal oxygen supply - oxygen alone is not enough - you need oxygen and AMP if you want to reconstitute the ATP supply.
OK, so the ribose treated dogs could make ATP. How does this rapid reconstitution of the ATP supply, as a result of ribose supplementation, affect cardiac performance?
Here we are looking at diastolic function, which is ATP dependent, but we could be looking at any biochemical reaction of importance to the heart; they are all ATP dependent. Diastolic function recovers rapidly in the ribose treated animals, because ATP regeneration recovers rapidly. Without supplemental ribose, ATP cannot be regenerated, so the heart remains stiff. We have only two studies of ribose supplementation in humans undergoing bypass surgery, but both demonstrated a benefit with ribose, and this only makes sense. It also makes sense that ribose would be of value in angina, CHF, and in athletes, which is the case. I have found ribose to be of great value to the patients I treat with EECP. These patients all have suffered from recurrent cardiac oxygen deficiency; all have a depleted adenine nucleotide pool and low levels of AMP. Even though we "re-oxygenate" these patients with EECP, until they can regenerate some AMP, they cannot use this "new" oxygen to make ATP. By supplementing my EECP patients with ribose, I have observed a more rapid and better sustained response to EECP - and doesn't this make sense?
.
James C. Roberts MD FACC
1/01/07
•