
| MME Fact Sheet |
|
Preparation & Nutritional Support |
| Abstracts and Publications | Upcoming Lectures | |
| Frequently Asked Questions | Contacting Us | |
| Policies of AMRI of NW Ohio | MME Home Page | |
| Messages from Dr. Roberts | Welcome Page |
No Longer Available
CARDIOVASCULAR OUTCOMES - Updated 8/06
The other MME centers focus on the use of MME in orthopedic and neurological conditions. My background is in Cardiology, and our medical practice, with its heavy involvement in EECP, focuses on the care of individuals with inoperable, recurrent, or treatment refractory cardiovascular disease states. Our MME program began in 9/04 - on this page I will present the outcome of every cardiovascular patient we treat over our 1st two years. We want you to know how we are doing, just as we did thirteen years ago when we brought EECP to town .
We got involved with MME specifically to help patients too-far-gone for our best current therapies and EECP. We are not utilizing MME as a substitute or replacement for standard cardiovascular care. Our cardiovascular patients either had recurrent disease, no longer amenable to revascularization, or their condition was such that revascularization would be associated with an increased risk - that is why they were treated with MME. Please remember, MME is not FDA approved. MME is considered to be an experimental therapy. Just because one patient gets better doesn't mean that another patient with similar symptoms will get better. Also, please appreciate that our patients received MME on top of the best standard and complementary cardiovascular treatment regimens that I could construct for them. MME applied as a "stand alone" therapy may certainly not lead to similar results. When it comes to the use of MME in cardiovascular disease, you need to understand that we are collecting outcome date on a still experimental therapy. Out goal is to learn how to best integrate MME into a comprehensive approach to the patient with cardiovascular disease, to learn the strengths and the limitations of this technique. As you scroll through the patient list, you will see how we have grown in sophistication in our application of MME, particularly with respect to the use of ancillary and supportive approaches.
While EECP is FDA approved to treat angina, coronary insufficiency, and heart failure, we are utilizing MME under the auspices of an IRB (Institutional Review Board). Scientific openness is important here. I'll divide this page into three sections, Angina and other symptoms due to Coronary Artery Disease, Cardiomyopathy and/or Congestive Heart Failure (CHF), and Other Conditions, acknowledging that there will be some overlap between these categories.
Angina and other Symptoms due to Coronary Artery Disease:
MME in
Post-Stent Placement Refractory Angina
MME to put a 85 year old Concert Violinist back in Coronary Tune - WR - 9/04
Angina, Atrial Fib, Nitric Oxide, Mercury, and MME - JR - 10/04
MME Thirteen Years Out from Bypass - BR - 12/04
MME for the ageing triathelete who can't catch his breath - RR - 9/04
Heart Failure, Liver Failure, and Inoperable Coronary Artery Disease - SD - 1/05
When bypass number two (25 years later) doesn't take - CM - 2/05
Too far gone for bypass in 2000 - BV - 2/05
EECP and MME for Acute and Chronic Coronary Insufficiency - CD - 6/05
EECP and MME for Refractory Symptoms following your 3rd bypass - DB - 6/05
Hearing Hoof Beats, Thinking Horses, and Missing the Zebra - KD - 9/04
Proactive Magnetic Cardiology - Taking MME to Prevent the Crisis - BP - 4/05
MME and EECP for Refractory Angina in a 92 year old Golf Enthusiast - RM - 7/05
Bringing back Memories - MME and EECP for the Heart and Mind - SP - 8/05
Two for One - MME for the Heart and the Lungs - JI - 9/05
EECP and MME following bypass and four rounds of stenting - ST - 9/05
MME in Inoperable Ischemic Cardiomyopathy - MJ - 10/05
MME for Coronary Disease and/or Cardiomyopathy - CE - 12/06
Cardiomyopathy and/or Congestive Heart Failure (CHF)
MME to help a Dilated Cardiomyopathy patient get back on his bike - BH - 9/04
MME for Chronic Dilated Cardiomyopathy - MV - 9/04
Cadmium, Cardiomyopathy, Cancer, and Hypertension - What's a Cardiologist to do? - HS - 12/04
Racing against the (Defibrillator) Clock - RD - 4/05
MME for Chronic Dilated Cardiomyopathy - BR - 11/04
Fixed and Vasospastic Ischemic Cardiomyopathy with Persistent Symptoms - SA - 10/04
Cardiomyopathy, Atrial Fibrillation, and Mitral Regurgitation - TM - 4/05
MME for Progressive Cardiomyopathy - SM - 10/05
55 Pounds of Edema Fluid lost in 25 days - HR - 5/06
A Big Man with a No Longer Big Heart - EN - 6/06
Helping a Runner to get Back on the Road - KD - 7/06
Cardiomyopathy and Hypertension (Lead) with Atrial fibrillation and a Recent CVA - DF - 11/06
Other Cardiac Conditions
Congenital Heart Disease with Hypertensive Heart Disease in and Adult - SH - 7/05
Sick Sinus Syndrome - Don't Stop Until the Job is Done - RH - 3/05
Carotid Disease, Non-dilatable Coronary Blockages, and SAD - BR - 11/05
Atrial Fibrillation and Single Vessel Occlusive Coronary Artery Disease - MG - 7/06
MME in Post-Stent Placement Refractory Angina
|
DATE |
EVENT |
| 4/00 | Initial Heart Attack → Angioplasty with Stent placement to occluded Circumflex; 50% LAD left intact and 70% & 95% distal RCA narrowings not dilatable |
| 7/00 | Unstable Angina due to Circumflex 90% in-Stent restenosis → repeat Angioplasty and Stent placement to Circumflex (creating a "Stent Sandwich") |
| 2/01 | Recurrent angina with an abnormal 4:44 stress echo study |
| 9/02 | Abnormal 2:52 stress echo - Nanobiotic therapy poorly tolerated ® 1/03 angiogram |
| 1/03 | LAD 50%, Circumflex stent open, with non-dilatable distal RCA narrowings |
| 12/03 | Unstable angina - new 80% LAD narrowing dilated and stented |
| 1/04 | Increased angina - both LAD and Circumflex stents open; multiple non-dilatable distal Right Coronary Artery narrowings again noted |
| 9/04 | 100 hours MME - angina resolved, meds decreased, & diastolic function improved |
| 6/06 | Coronary Angiogram - No significant change from 1/04 |
I've worked hard to control CR's angina, or perhaps we should say that I worked him over hard. Still, CR's symptoms did not come under control until he was treated with MME - here's CR's story:
This 65 year old hypertensive, hyperlipidemic, diabetic man with sleep apnea and several additional coronary risk factors presented with severe chest pain in 4/00. CR was in the midst of a heart attack, due to occlusion of his Circumflex coronary artery, which supplies the side wall of the heart. The Circumflex was dilated open with a balloon catheter, and then stented. High-grade narrowings were seen in the RCA (Right Coronary Artery), but they were located at its distal extent, beyond a bend, and beyond the reach of the angioplasty catheter. The LAD (Left Anterior Descending), which supplies the front wall of the heart, contained a non-flow restrictive 50% narrowing, and was left intact.
CR felt great for three months. Then chest pain recurred, and angiography demonstrated renarrowing within the Circumflex stent, termed in-stent restenosis. The Circumflex narrowing was re-dilated and a 2nd stent was placed within the 1st one, creating a "stent sandwich". CR's angina improved with this procedure, but it did not fully resolve. A stress echo study showed the problem to be insufficient blood flow to the heart muscle supplied by the RCA, which contained 70 & 95% narrowings that could not be angioplastied or stented. CR was put on an extensive nutritional program, diet and drug therapy for sugar control, and as much anti-ischemic drug therapy as he could take, including 200 mg/day of the b-Blocker Metoprolol, but his symptoms did not resolve. Nanobiotic therapy was tried, and helped a little, but CR couldn't tolerate this treatment long-term. Angiography in 1/03 (CR's third) showed the stent sandwich to be open, the LAD to be unchanged, and the same high-grade narrowings in the distal RCA.
11 months later, in 12/03, CR's chest pain flared up - the LAD narrowing now involved 80% of the vessel's flow area; the LAD was dilated and a drug-eluting stent placed. Three weeks later I had to repeat CR's heart cath, due to persistent pain. The LAD stent site was open, but when I injected X-ray dye into this vessel, CR experienced severe angina (The problem here was endothelial dysfunction, an inability of the artery lining endothelial cells to generate Nitric Oxide. Without Nitric Oxide the vessels cannot dilate properly and resist platelet aggregation or vasospasm. Endothelial dysfunction persists for up to 6 months post-procedure in a stented artery.). Multiple pharmacologic and nutritional therapies aimed at endothelial dysfunction were tried, but none got the job done. CR's angina worsened in 1/04, and angiography, CR's 6th, demonstrated a wide open LAD stent site, a moderate, certainly non-critical narrowing of the Circumflex stents, and the high grade RCA narrowings observed on all prior studies. I felt that CR's persistent pain was due to persistent endothelial dysfunction, and to persistent oxygen starvation in the heart muscle supplied by the diseased (and non-dilatable) RCA. A cardiac echo study demonstrated findings of CR's initial heart attack, along with evidence of of diastolic dysfunction (CR's heart was stiff and filled poorly, making him short of breath with effort). CR needed at least two NTG tabs each day and basically felt like hell - as did I, because it was my job to help him, and all I seemed to be able to do was to try different drugs and then carry out heart catheterizations on CR, over and over.
CR has a background in engineering, and he understands electricity and magnetism better than I do. I, on the other hand, understand cardiovascular physiology better than CR. When MME became available in Toledo, we put out heads together and decided that MME might just be able to get the job done, the job that I hadn't completed despite 6 heart caths, three rounds of stenting, and the 8 drugs and 19 different nutritional supplements that I had CR on.
In preparation for MME, CR began sleeping on a 10 Gauss Magnetico negative field sleep pad. At bedtime, every other night, he took DMSA (a metal binding agent). CR did not experience a reduction in angina, but with this simple maneuver his energy level picked up a little, and his long-standing leg aching let up a little. Then we began MME - during the first few sessions, CR noted a strange sensation in his chest - not his angina, not shortness of breath, but more of a tingling sensation. After 45 hours, CR felt he "turned the corner". CR could do more, and he no longer required oxygen during light exercise. CR's improvement continued and we stopped at 100 hours. A post-MME cardiac echo study showed CR's heart to be less stiff (consistent with an improvement in cellular energy generation). Before we started MME, CR would experience angina with daily activities and occasionally at rest. Now CR can work without difficulty; angina has resolved, NTG is no longer needed, and we were able to decrease CR's Metoprolol dose from 200 to 100 mg/day. CR's functional status has thus improved in a meaningful fashion. CR will continue to sleep on the Magnetico sleep pad, and will take DMSA at bedtime 7 days a month.
1/06 Update - CR remains improved, and has not required a hospital stay or invasive study since completing MME in 9/04.
7/06 Update - In 6/606 CR noted recurrent chest tightness and increased shortness of breath with effort; his weight had increased and we couldn't tell whether his symptoms were weight related or due to progressive coronary disease. Angiography revealed a stable situation, to my eye unchanged from CR's 6th heart study in 1/04. CR is going to work on weight and sugar control. CR's Testosterone level is low (a nearly universal finding in male patients with coronary disease). 1400 mg of Testosterone in pellet form was implanted subcutaneously in 7/07. Testosterone dilated coronary vessels, promotes clot dissolution, improves insulin sensitivity, and provides a number of other benefits for the cardiovascular patient, and hopefully will reduce CR's symptoms. The good news is that his coronary disease remains in check.
MME to put a 85 year old Concert Violinist back in Coronary Tune - WR - 9/04
|
DATE |
EVENT |
|
7/02 |
Coronary calcium score 891 with a normal 5:00 stress echo |
|
7/03 |
New onset angina → angio with high-grade, not-dilatable narrowings in the marginal branch of the RCA and in 2 of the 3 marginal branches of the Circumflex. |
|
8/03 |
35 hours EECP with a full resolution of angina |
|
9/04 |
Fatigue, palpitations, edema, and shortness of breath with effort → 150 hours MME |
|
11/04 |
Symptoms improved to resolved, with a negative 5:34 stress echo study |
I've been working with WR for 5 years, helping this now 85 year old, incredibly energetic concert violinist with high blood pressure, cardiac arrhythmia (SVT and intermittent atrial fibrillation), edema, and postural dizziness. WR did not tolerate pharmaceutical therapy well, so I had her on only two drugs, but she had been doing well on an incredibly complete and incredibly energetic nutritional program. Mercury overload had been demonstrated and to some degree addressed, and with this her arrhythmia and postural dizziness became easier to control.
A screening coronary artery CT calcium study returned abnormal in 7/02, but WR could complete 5:00 on the treadmill and her stress echo images looked good. Anginal chest tightness developed one year later, and WR's angiographic study demonstrated high-grade narrowings in three major branch vessels, positioned beyond the reach of the angioplasty catheter. EECP was carried out, along with additional anti-atherosclerotic measures. WR did well, and returned to the concert hall and her busy lifestyle.
WR felt herself slowing down, and slowing down fast, in the fall of '04. Shortness of breath was shortening her daily swims and she had no energy. Postural dizziness was more of an issue. I felt that coronary insufficiency was the culprit. We discussed repeat EECP, or a repeat angiogram, looking for a new narrowing that might be the culprit. WR was aware of MME and its potential benefits, and she chose MME over repeat angiography. This turned out to be a good decision.
WR kept a detailed symptom diary during her MME. She noted a gradual improvement in her energy level, and soon she could complete her morning swims without difficulty. Dizziness and palpitations became non-issues. Her 5:34 stress echo study looked great. WR noted a number of non-cardiac benefits. A lipoma on her left arm decreased in size. Pre-MME she was experiencing a tremor when she picked up her violin - this went away and her arthritis also seemed a little better. We treated WR's heart, not her entire body, so its a little difficult to explain her non-cardiac improvements. It may be that by magnetizing the blood as it passes through the heart that we are magnetizing the entire body, or maybe a stronger heart does a better job of supplying energy to the other internal organs. WR doesn't much care that I can't explain why she is better. She's just happy to be better (and by the way, if her concert performance improves, I'm going to take full credit)!
Addendum: Now that WR is doing more, arthritic knee pain is becoming more of an issue. Knee replacement would solve this problem. She might get some relief from the Viox-type drugs (scratch that - bad idea). Our approach, before we resort to drugs or surgery, will be to treat WR's knees with MME.
7/06 Update - WR remains improved; chest pain has not recurred and WR has experienced only a single, brief episode of atrial fibrillation since completing MME in 9/04. She has not required a hospital stay or invasive study.
Angina, Atrial Fib, Nitric Oxide, Mercury, and MME - JR - 10/04
|
DATE |
EVENT |
|
3/94 |
LAD angioplasty with restenosis, leading to LIMA to LAD bypass surgery |
|
7/94 |
Anastomotic lesion, leading to angioplasty of the LAD and diagonal |
|
7/97 |
Rotablation and stenting of the Circumflex |
|
7/97 |
Atrial Flutter developed and responded to electrical cardioversion |
|
3/98 |
Circ restenosis with Class 4 angina despite four drug medical therapy |
|
4/98 |
35 hours EECP ® Class 1 functional status, 2 drugs dropped, and angina minimal |
|
4/99 |
20 hour EECP booster for Circ distribution ischemia |
|
8/99 |
Increased angina - new 80% marginal narrowing that was dilated and stented, LIMA and proximal LAD and diagonal patent, Circ occluded, and distal 90% LAD |
|
11/99 |
Marginal restenosis, addressed with repeat angioplasty and stent placement |
|
2/00 |
Class IV angina, resolved with 45 hours EECP |
|
10/00 |
Angina - Arteries unchanged: Circ 100% with distal LAD 90% - marginal open |
|
11/00 |
38 hours EECP with again a resolution of angina - 10 hours given in 4/01 |
|
11/01 |
Atypical pain - arteries without change from 10/00 - no disease progression |
|
6/02 |
EECP booster and EDTA and Nanobiotic therapy ® angina resolved |
|
3/03 |
EECP booster and again in 8/03 |
|
12/03 |
Angina - arteries unchanged from 10/00 and 11/01 |
|
2/04 |
EECP booster |
|
7/04 |
Pneumonia, precipitating Atrial Fib-Flutter; drug therapy decreased HR excessively |
|
10/04 |
Angina with low HR requiring pacemaker implantation Þ Instead 35° EECP - this time with 150 ° MME with DMSA |
|
12/04 |
Angina resolved, anti-arrhythmic drug stopped and rhythm stable, with an only mildly abnormal 8:00 stress echo study ® sleep pad and cyclic DMSA |
|
2-3/05 |
EECP booster and 150 hours of MME with DMSA |
|
7/05 |
Feels great - no angina and rhythm stable |
Isn't this a rather long problem and procedure list? JR is one of our favorite patients. Each year the staff invites him to the office Thanksgiving lunch. We should, as JR basically paid for the place. JR's case study has been presented previously on this website (EECP case history #6), as in 4/98 JR did well with EECP, after undergoing 5 heart caths, bypass surgery, and three angioplasty/stent procedures, all in the space of 4 years.
JR did do well with EECP in mid-98; his chest pain resolved and his stress study improved. Angina recurred one year later, and his stress study pointed to ischemia (evidence of insufficient blood flow) in the heart muscle supplied by the occluded Circumflex. I felt his collaterals needed boosting; a booster course of EECP was carried out, and JR again felt well. A new narrowing developed in JR's marginal artery in 8/99. This vessel was dilated and stented, but just as with JR's LAD, the stent closed and a repeat procedure was required 3 months later.
Between late '99 and the present, JR's course has been marked by angina flare-ups every 6 months, each time with a good response to EECP. EECP works not just be augmenting collateral flow. EECP doubles your Nitric Oxide level; this is the angiochemical that dilates your arteries and allows them to resist spasm and platelet clotting. When you take a NTG, what you are really doing is giving your circulation a jolt of Nitric Oxide. JR would do well with EECP, but then the effect would wear off and I'd have to treat him again. My feeling was that some toxin, probably a heavy metal, was producing oxidative stress, basically "chewing up" JR's Nitric Oxide, such that he needed EECP every 6 months to "top up" his Nitric Oxide tank. All along JR had been on a program of antioxidant vitamins and fish oil; we redoubled our efforts and JR began a program of IV EDTA chelation therapy to remove what I thought to the the culprit heavy metals, and JR received several months of Nanobiotic therapy, which also provides EDTA. JR's Mercury amalgam fillings were removed in 2001, but this was not accompanied or followed by any specific medical Mercury detoxification (a big error on my part). These measures have kept JR out of trouble, in that he has never experienced a heart attack, and I think he has had only 2 unplanned cardiac hospital admissions in the last 5 years, but we have not kept JR out of the cath lab, and we have not kept JR pain free.
JR had developed Atrial Flutter in '97; this rapid atrial arrhythmia precipitated angina but fortunately responded to electrical cardioversion. JR was hospitalized with pneumonia in 7/04, and this infection precipitated another episode of atrial arrhythmia. Drug therapy converted JR's rhythm back to normal, but only at a very slow rate. Consequently I had to back off on JR's b-Blocker dose, as this agent works by lowering the heart rate, but then his angina flared up. This was a dilemma. The drug therapy for arrhythmia was working, but slowed JR's heart rate too much, compromising his angina treatment program. The solution was to place a cardiac pacemaker, but a pacemaker would close the door to MME forever - what to do?
I struggled with this one. First I needed to ask: What was I missing? What should I have done to help JR hold on to his Nitric Oxide and remain angina free? What was causing the nerves in his heart to malfunction? We had done everything right. We had done everything we could - except one thing, one very big thing. JR had had his Mercury amalgams removed, but he had never undergone any medical Mercury detoxification. Could Mercury be the toxin chewing up JR's Nitric Oxide? Could Mercury be poisoning JR's cardiac nerves? This hypothesis made sense to me, so I presented JR's case to Dr. Bonlie. JR received a booster course of EECP, to increase the cardiac blood supply and re-generate his Nitric Oxide pool, and he began MME, coupled with oral DMSA Mercury detoxification therapy, aiming to remove Mercury from JR's heart.
JR noticed a "tingle" during his initial MME treatments. At 25 hours he noted a reduction in angina frequency and severity. At 50 hours I began to cut back the dose of JR's anti-arrhythmia drug, and at 100 hours this rhythm control agent was discontinued. Following this EECP booster, coupled with 150 hours of MME, JR feels great, his heart rhythm is normal, and his energy is back. Post-MME JR has experienced only one episode of angina, and that was when I ran him into the ground on a 8:00 stress echo study, which returned only mildly abnormal (his Circumflex is 100% blocked and you can always outstrip the collateral blood supply if you push exercise hard enough, which we did here for diagnostic purposes). JR will sleep on a Magnetico sleep pad and take DMSA on a periodic basis (to keep pulling Mercury and other toxic metals out). Given JR's history, I won't declare victory, not just yet, but he's sure feeling better following MME, and so am I, as I'm the guy who put him through 10 heart catheterizations, bypass surgery, and 5 rounds of angioplasty/stent placement. Let's hope I got it right this time.
JR had the following comments about his MME experience - "My heart is beating stronger than it was before I started MME. Before, my pulse was always low and now it's always in the 60-70's. Even though the 7-days-a-week regimen was at times trying, the ongoing results were encouraging. Now that I'm done and feeling as good as I do, the extra effects and cost make it worthwhile. Overall I'm feeling the best I have felt in several years".
7/05 Update - To be on the safe side, given JR's history of recurrent coronary insufficiency, he received an additional 150 hours of MME with a concomitant EECP booster in 2-3/05. As of 7/05, JR feels great. Angina has not recurred and his rhythm remains normal.
7/06 Update - JR's Atrial Flutter recurred, increasing his heart rate and with this angina recurred. Trans-catheter flutter ablation was carried out, and with this JR's angina resolved. Atrial flutter recurred, and again responded to flutter ablation. A sinus infection put JR back into flutter; cardioversion is planned. I have not repeated JR's coronary angiogram as I feel that the problem is the recurrent atrial arrhythmia, not coronary disease progression. JR tolerates the flutter reasonably well, but it does bring on angina. When in normal rhythm JR is angina free.
MME Thirteen Years Out from Bypass - BR - 12/04
|
DATE |
EVENT |
|
2/92 |
Inferior wall heart attack |
|
2/92 |
Bypass surgery for Left Main and 3 vessel coronary disease |
|
9/99 |
Mild angina with an abnormal 9:00 stress echo - medication responsive |
|
11/00 |
Mildly abnormal 7:35 stress echo |
|
8-12 '01' |
Recurrent symptoms ® 4 months of Nanobiotic therapy with a decrease in angina, decrease in coronary artery calcium score from 3240 to 2754, with a still abnormal but improved 8:47 stress echo |
|
4-8 '03 |
Recurrent angina, responsive to 20 rounds of DeToxMax Plus |
| 9/04 | Shocking news ® unstable angina ® All 3 grafts widely patent but the 50% Left Main narrowing was compromising flow to proximal LAD and Circ distributions |
| 10-12 '04 | 45 hours EECP - symptoms improved but not totally resolved |
| 12/04 | 104 hours of MME ® Angina fully resolved and meds decreased |
| 6/05 | Remains angina free with a normal 7:00 stress echo |
MME is a therapy that we had been looking for, a technique that could help patients who were not responding well, or responding completely well, to our prior best therapies. Our best therapies had kept BR's grafts open for 13 years, but hadn't totally resolved his pain, and this man with an upcoming challenge to his non-cardiac health needed something more.
BR Presented in 2/92 with a heart attack involving the back wall of his heart. Angiography demonstrated narrowings within the Left Main and all three of BR's major coronary vessels, leading to three conduit bypass surgery. Angina recurred 7 years later, in association with an abnormal stress echo study, and quieted down nicely with anti-anginal drug therapy. BR's stress echo study 1 year later was a little worse, and angina returned in the fall of '01. BR received 4 months of Nanobiotic therapy; angina lightened up, and BR's stress echo and coronary calcium scores improved. BR's symptoms returned two years later, and quieted down nicely with 20 weeks of DeToxMax Plus. Things went well until the fall of 2004, when BR was broadsided by a confluence of stressful events.
One piece of bad news, or one stressful event, may effect the blood pressure and coronary tone of any patient with coronary artery disease. BR experienced three such stressors, the most important one pertaining to a non-cardiac health issue. His BP soared to 231/114, his arteries clamped down, and I had to admit him to the hospital with troponin positive unstable angina. Angiography demonstrated that all three of his 13-year-old bypass grafts were widely patent, while the 50% Left Main narrowing was compromising flow to the muscle in the LAD and Circumflex distributions proximal to their occlusion and subsequent graft insertion points. I increased BR's drug doses; this helped a little, but not a lot, and also led to fatigue, something BR didn't need.
In thinking about BR, first I was rather pleased with the work that BR and I had done. One in three bypass grafts close the 1st year and 50% of vein grafts close down by 7 years, but all 3 of BR's 13-year-old grafts looked good. However, he still had pain, the meds were causing fatigue, and it was my responsibility to get BR in tip-top shape, to help him deal with an important non-cardiac health challenge.
So, BR underwent EECP, and that helped, but did not totally resolve his angina. EECP was followed by MME, and this did. During MME I was able to cut down on BR's medical regimen, aiming to give him more energy, which he will need in the near future. A stress echo study is planned to serve as a new baseline, and we will continue the treatment programs that have protected BR's grafts over the past 13 years.
7/06 Update - Following completion of EECP and MME in 12/04, BR underwent a medically stressful therapy for a non-cardiac health condition - and he did great. A 7:00 stress echo study carried out in 6/05 looked good. Angina recurred when out in the cold in early '06. A booster course of EECP was carried out, and as of now BR is pain free and feeling well.
MME for the ageing
triathelete who can't catch his breath - RR - 9/04
|
DATE |
EVENT |
| 6/93 | Normal 18:00 stress echo |
| '94 | Atrial fibrillation, responsive to medical/nutritional therapy |
| 11/98 | 14:42 stress echo with an equivocal fixed inferior wall contraction abnormality |
| 4/04 | Shortness of breath with effort - Obviously abnormal 13:00 stress echo with a resting inferior abnormality that worsened with exercise Þ |
| 5-6/04 | 35 hours EECP |
| 4-8/04 | Magnetico negative field sleep pad and oral DMSA |
| 9/04 | 150 hours MME |
| 10/04 | Symptoms - Fully resolved; can play singles tennis without difficulty Stress echo - Contraction abnormality post-exercise worse but treadmill time increased to iiiincreased to 15:00 minutes |
| 12/04 | Silver Protein vs. infection, Phosphatidyl Choline for reverse cholesterol transport, with ongoing DMSA/sleep pad therapy ® more MME this winter |
| 3/05 | 100 hours of MME |
| 4/05 | Running again - On no drugs and without a care in the world |
| 4/05 | 15:00 stress echo with a mild resting abnormality that doesn't worsen post-exercise |
| 9/05 | Normal cardiac echo - Inferior wall contraction abnormality no longer present |
Coronary disease is not a condition one would expect in RR, but that was the diagnosis facing us last spring, when this 76 year-old semi-retired physician, a former marathon runner, was facing retirement from the tennis court. A life-long athlete, RR's heart rate had always been low, and his EKG was unusual in appearance (related to athleticism). This prompted a stress echo study for insurance purposes in mid-'93. RR burned it up, running for 18:00, just as do high school athletes undergoing sports physicals.
Atrial fibrillation developed in '94. Digoxin, Co-Enzyme Q10, and Carnitine were added to RR's nutritional program; the atrial fib resolved and to this point has not returned. A screening stress echo study in late-'98 demonstrated an equivocal contraction abnormality, at rest and with effort, over the back wall of RR's heart. Given that RR felt great and could complete 14:42 of treadmill stress, I felt that this represented artifact, as opposed to a small inferior wall heart attack (but in retrospect I was probably wrong). RR's risk factor profile looked great: LDL 102, Lp(a) 7, HDL 68, and fasting sugar 86. His homocysteine was a little high at 13.7, but fell with B-vitamin supplementation. RR was maintained on a program of antioxidant, mineral, and essential fatty acid supplementation, and he continued to exercise on a regular basis, and to exercise without difficulty.
RR continued to feel great until the spring of '04, when he began to experience shortness of breath with physical activity. Hunting was a little more difficult; singles tennis was a real strain. A 13:00 stress echo showed an inferior wall contraction abnormality at rest, that definitely worsened with effort. Coronary disease was the obvious culprit - what were we to do next? RR's heart rate and blood pressure remained low, from his athleticism, such that anti-ischemic drug therapy would likely due more harm than good. It didn't make sense to me to subject a 72 year-old who could walk for 13:00 on the treadmill (it is unusual for a 70 year-old to even go 6:00) to angioplasty or bypass surgery, so we decided not to carry out an angiogram. I also needed to come up with an explanation(s) as to why an athletic man with no standard risk factors was being troubled by coronary insufficiency in the first place, so that I could include coverage for those potential culprits into my overall treatment plan for RR.
We are learning that heavy metal overload (probably Mercury more than Arsenic, Lead, and Cadmium), is playing a role in our current rising epidemic of coronary artery disease. These metals poison our antioxidant and reverse cholesterol transport systems, and many other enzyme systems as well. Chronic, smoldering infection, as well as one's life-time "infectious burden" also play key role's (infectious burden correlates with one's CRP level, and with this one's risk of coronary disease and coronary events - the relationship is stronger than the relationship between cholesterol and heart disease). RR's Mercury amalgam fillings were removed in '01; subsequently he had then received 5 IV DMPS (Mercury binder) treatments, decreasing his post-DMPS urine Mercury level from 23 to 8 mcg Hg/G creat. An IV EDTA challenge study had returned abnormal for Lead at 43 mcg/24 hours. These were not particularly alarming levels, so I had not pushed RR into a more aggressive or ongoing metal removal program (another mistake on my part).
Aiming to address these potential culprits as we resolved RR's symptoms, the following program was initiated:
1. RR began to sleep on a 20 Gauss Magnetico negative field sleep pad, taking DMSA 500 mg at bedtime every other evening, aiming for a low-level total body magnetic energizer effect and enhanced metal detoxification.
2. 35 hours of EECP were carried out.
3. RR received 150 hours of MME in 9/04.
With these measures RR's symptoms fully resolved. He is back on the tennis court, and he can hunt and fish without any limitation. A follow-up stress echo study was obtained. The exam was stopped at 15:00, not because RR felt poorly, but because he had reached his target HR; he feels he could have gone farther. Post-exercise wall motion, however, looked worse than on RR's pre-treatment study. Viewed out of context, this would suggest that RR was worse. However, given that RR's symptoms had resolved, wall motion may be more abnormal because RR was able to push himself farther. It really doesn't make sense to me that an individual whose symptoms have resolved and whose treadmill time has increased could actually be worse, and again, I couldn't see operating on an asymptomatic 76 year-old who can run for 15:00, so we continued out conservative approach.
4. RR began a program of IV Phosphatidylcholine. This material stimulates LCAT (Lecithin Cholesterol Acyl Transferase), the key HDL-associated enzyme that mediates reverse cholesterol transport (this enzyme is inhibited by heavy metals).
5. RR began MSP (Modified Silver Protein - blocks oxygen utilization in unicellular microbial invaders but leaves multicellular organisms like us alone), aiming to decrease his infectious burden and blunt inflammation.
6. Antioxidants, minerals, essential fatty acids, along with Co-Enzyme Q and carnitine will remain on board, and RR continues to exercise.
7. This winter, when it is too cold outside for RR to go hunting, he will undergo additional MME.
RR described his MME experience as follows:
"I undertook 150 hours of MME treatment for coronary artery narrowing. The 12 hour periods during the night were almost enjoyable - four hours of reading and for TV and eight hours of sound sleep. My score on the Bruce Protocol stress challenge increased from 13 to 15 minutes - maximal for my age. More important was my ability to beat my old tennis competitor by playing a full 90 minutes without needing the breathing breaks required before MME.
Happily I never experienced chest pain, just shortness of breath and easy fatigue, before MME corrected that - and I trust will prevent any chest pain angina in the future".
Summer '05 update: RR received an additional 100 hours of MME in March. He has returned to running (no marathons - he leaves those to his kids). RR is not taking a single cardioactive prescription drug. He will keep up with the Magnetico sleep pad, a nutritional program, oral phosphatidylcholine, and periodic oral DMSA.
Fall '05 update: RR feels great - his cardiac echo study is now normal - wall motion is normal, the ejection fraction is normal, and diastolic function is normal - the inferior wall contraction abnormality observed on RR's prior studies has resolved. RR has not undergone angiography, but his clinical presentation, resting echo, and stress echo studies point to coronary artery disease (prior inferior wall heart attack with additional heart muscle at risk) as the culprit. Following RR's initial 150 hours of MME, his symptoms resolved, but RR's stress echo study, obtained as he finished the 150 hours, remained abnormal. Six months later, and following an additional 100 hours of MME, RR's stress echo study was normal - that is, there was no evidence for additional heart muscle at risk - but the resting inferior wall contraction abnormality, reflecting a prior heart attack, was still present. Now, one year out from RR's initial MME, resting wall motion is unequivocally normal.
What does this time course mean?
It means, in my opinion (and I can't be sure of any of this - these are just my thoughts), that cardiac healing brought on by MME occurs slowly, initially at the molecular level, and then at the biochemical level. Later, the blood vessels change, and only late after MME, in RR's case 12 months, do we see a change in the appearance of the heart. Early on, MME is probably generating ATP energy, improving function at the cellular level - RR could do more, early on post-MME, as his cells had more energy. Collateral vessels were likely functioning more efficiently, as static magnetic fields regenerate Nitric Oxide. RR was back on the tennis court, but his stress echo remained abnormal, likely because, in this limited time frame, not enough time had elapsed for the biochemical changes induced by MME to change the diameter of his major coronary arteries. Six months out from MME, RR's stress echo study had normalized. This might be due to the additional 100 hours of MME that he received, or it may simply be that it took 6 months for his original 150 hours to affect the architecture of the arteries. We think that MME stimulates stem cells within an organ to proliferate and migrate. In RR, post-initial MME we saw, at least grossly by echo, no evidence that this phenomena was taking place; the same at 6 months - the dead muscle still looked dead. At 12 months, however, the area appears to have been regenerated. We probably need to be patient - it took our hearts 9 months to form up in the 1st place. Post-MME we probably need to allow the same time frame for the stem cells we stimulate to regenerate the cell population in a damaged region. Again, this is what I think is going on, based on my study of the literature and my analysis of how my patients are responding to MME. Time will tell if we are right - but right now RR is happy with the way his heart looks, and he is happy with his tennis game.
7/06 Update - RR continues to do well; he enjoys hunting, fishing, and hour-long tennis matches and remains asymptomatic.
Heart Failure, Liver Failure, and Inoperable Coronary Artery Disease - SD - 1/05
SD had three otherwise untreatable health problems, so she came to see us for MME and EECP. This 70 year old woman with medically addressed hypertension and diabetes was diagnosed with advanced liver dysfunction in 1993. Her liver was fibrosed and scarred (termed cirrhosis), compromising its ability to clear toxins from the blood and leaving her with an impossible to treat lipid abnormality. Blood draining from the GI tract "damned up" behind the liver, producing esophageal varices. The esophagus is the swallowing tube that connects the throat with the stomach. Think of esophageal varices as varicose veins within the esophageal wall. They don't trouble you - that is until they rupture, producing life-threatening hemorrhage (when I was an intern, I would stay up all night trying to keep esophageal "bleeders" out of shock). The cause of SD's liver dysfunction was never determined. Viral studies returned negative and SD does not consume alcohol; her gastroenterologist could not determine the cause and he had no treatment options to give her.
One year ago, SD began to experience angina, chest pain on the basis of impaired coronary artery blood flow, and shortness of breath with effort, due to impaired cardiac pump function. Given SD's liver problems, her physicians initially tried to treat her with medications, but her symptoms unfortunately progressed. Angiography carried out in the fall of '04 revealed occlusion of two coronary arteries (the Left Anterior Descending and Marginal) and a 90% Right Coronary Artery narrowing. Only one artery, the Circumflex, remained open. Two heart attacks had occurred, compromising heart pump function. Normally a 70 year old with this pattern of blockage would be treated with bypass surgery, but in SD's case, the anesthetic and bleeding risks would be astronomical, and she was turned down for bypass. Despite an extensive drug regimen, SD was experiencing 2 episodes of angina each day, requiring 5-10 NTG tablets per week. SD lives in Southern Ohio but she has family in the Toledo area, so she came up to see us.
To effectively treat SD, I had to effectively treat three problems at once - SD has to be the most complicated patient I have ever taken care of. My plan was to treat SD simultaneously with a program of EECP, MME, nutritional support, and detoxification. EECP was initiated in early 12/04, followed by MME (with oral DMSA), 2 hours each day to the liver and 2 hours each day to the heart, in early 1/05 (our first opening). Her prior medications were continued, and I added N-Acetyl Cysteine, Silymarin, and Lipoic Acid (liver protective nutritional agents).
Angina-wise this program worked; SD's chest pain fully resolved and NTG is no longer required. SD's blood pressure was under great control on medications, with a pre-treatment value of 120/80. Her BP fell further as a result of our treatments (as blood vessels dilated your BP can fall); this led to dizziness, prompting a decrease in her diuretic (water pills) and vasodilator drug doses. This proved to be an error on my part, as off these agents SD's heart failure flared up. We recognized the problem, resumed several of her medication, and with this her heart failure symptoms quieted down. SD's cardiac echo findings did not improve; advanced pump dysfunction and significant regurgitation behind her mitral valve were present before and after our treatments, but perhaps we need to be a little patient here, and not expect anatomic changes in just a few weeks.
 In patients with kidney disease, we monitor serum Creatinine as an index of
kidney function. Creatinine is generated by our muscles at a constant
rate and is cleared from the body via the kidney. If kidney function
falters, or if you become dehydrated, the serum creatinine will rise. If
kidney function improves, the creatinine level will fall. Clinically we
use the serum creatinine to guide our medical treatments for heart failure.
The liver also filters the blood, retaining desirable blood products and
clearing wastes into the bile. Clinically we use the serum Bilirubin
level as a marker of liver function. A normal Bilirubin is < 1.3 mg/dL.
SD's pre-treatment Bilirubin was elevated, 2.3 in 9/04 and 3.1 in late 11/04.
One week into MME her Bilirubin value was 2.6, suggesting an improvement in
liver function, but one week later her Bilirubin was 3.4, above the
pre-treatment value. SD didn't feel worse, but this rise in SD's
Bilirubin sure had we worried - was I helping her or hurting her? Dr.
Bonlie was not worried. He has seen this phenomena before when MME is
used to treat advanced liver disease; he sees the Bilirubin rise, and then
fall. His theory is that Bilirubin "stuck" within damaged liver cells is
released as the cells regain their function. He may cut back on the
number of hours each day that the patient is treated with MME, but he never
stops, and the Bilirubin always falls back over time. We had the same
experience with SD. Advanced heart failure is typically treated with 200
hours of MME, and liver failure requires the same duration of MME treatment,
but with SD we stopped after 50 hours to the heart and 50 hours to the liver.
We stopped early because SD's primary problem, inoperable angina, had resolved
and she needed a break as she had been away from home for nearly two months.
Two weeks out from MME SD's labs were repeated and I spoke with both SD and
her primary physician. SD was feeling well; angina had not recurred, and
her breathing had improved further, and her Bilirubin had fallen to 2.5 - Dr.
Bonlie was right. After SD has rested up, our plan will be for her to
return to Toledo for further MME to her heart and liver. SD's care is
still "a work in progress:, but so far things are certainly going her way.
In patients with kidney disease, we monitor serum Creatinine as an index of
kidney function. Creatinine is generated by our muscles at a constant
rate and is cleared from the body via the kidney. If kidney function
falters, or if you become dehydrated, the serum creatinine will rise. If
kidney function improves, the creatinine level will fall. Clinically we
use the serum creatinine to guide our medical treatments for heart failure.
The liver also filters the blood, retaining desirable blood products and
clearing wastes into the bile. Clinically we use the serum Bilirubin
level as a marker of liver function. A normal Bilirubin is < 1.3 mg/dL.
SD's pre-treatment Bilirubin was elevated, 2.3 in 9/04 and 3.1 in late 11/04.
One week into MME her Bilirubin value was 2.6, suggesting an improvement in
liver function, but one week later her Bilirubin was 3.4, above the
pre-treatment value. SD didn't feel worse, but this rise in SD's
Bilirubin sure had we worried - was I helping her or hurting her? Dr.
Bonlie was not worried. He has seen this phenomena before when MME is
used to treat advanced liver disease; he sees the Bilirubin rise, and then
fall. His theory is that Bilirubin "stuck" within damaged liver cells is
released as the cells regain their function. He may cut back on the
number of hours each day that the patient is treated with MME, but he never
stops, and the Bilirubin always falls back over time. We had the same
experience with SD. Advanced heart failure is typically treated with 200
hours of MME, and liver failure requires the same duration of MME treatment,
but with SD we stopped after 50 hours to the heart and 50 hours to the liver.
We stopped early because SD's primary problem, inoperable angina, had resolved
and she needed a break as she had been away from home for nearly two months.
Two weeks out from MME SD's labs were repeated and I spoke with both SD and
her primary physician. SD was feeling well; angina had not recurred, and
her breathing had improved further, and her Bilirubin had fallen to 2.5 - Dr.
Bonlie was right. After SD has rested up, our plan will be for her to
return to Toledo for further MME to her heart and liver. SD's care is
still "a work in progress:, but so far things are certainly going her way.
7/06 - SD had maintained her gain after returning home. She did not required any hospital care or significant change in her program of medications. SD passed away, rather suddenly, from a kidney/urinary tract infection that spread into her blood stream
When Bypass Number Two (25 Years Later) Doesn't Take - CM - 2/05
|
DATE |
EVENT |
| 9/79 | Inferior Wall Heart Attack |
| 1/80 | Bypass surgery to RCA and Marginal - LAD and Circumflex wide open |
| '92 | Two rounds of angioplasty to the Circumflex |
| 9/92 | Open grafts to the RCA and Marginal with LAD 95% and collateral filling of the LAD |
| '97 | Recurrent angina ® 45 IV EDTA treatments |
| 1/02 | Effort angina with an abnormal 9:48 stress echo |
| 8/02 | Angina improved following 4 months of Nanobiotic therapy |
| 6/04 | New CHF - Ejection Fraction 25-30% ® Increased medical therapy |
| 6/04 | High grade Left Main and LAD narrowings, 95% narrowing in the SVG to occluded RCA with occlusion of the Circumlex and its graft 100% |
| 7/04 | LIMA to LAD and SVG to Diagonal and RCA |
| 9/04 | Normal 6:40 stress echo - resting EF 40-45% |
| 12/04 | Recurrent angina with a + 13:35 (modified protocol) stress echo - resting EF 30-35% and post-exercise EF 30-35% |
| 1-2/05 | 45 hours EECP and 100 hours MME |
| 3/05 | 14:00 (modified protocol) stress echo without angina - resting EF 40-45% and post-exercise EF 50-55% |
| 6/05 | Resting EF now normal, with less mitral regurgitation |
CM is 25 years out from his original bypass surgery; he is a unique gentleman and I really enjoy working with him. I have one other patient in my practice who is alive 20 years out from bypass surgery, but I've never heard of anyone being physically active 25 years following their bypass. CM has obviously done an excellent job taking care of himself. He's learned a lot and applied these principles to his own health. CM has some strong opinions, and our minds don't always meet; usually he gets his way (should I be arguing with success?), but occasionally I prevail. I pushed CM hard to undergo a second bypass in the summer of '04, and felt bad when it didn't take. Fortunately we were able to rectify the situation with EECP and MME.
CM sustained a small heart attack in '79. The Right Coronary Artery and the Marginal branch of the Circumflex were blocked, and received bypass grafts in '80. The Left Anterior Descending and Circumflex were disease free in '80, but over the years accumulated plaque, such that two rounds of angioplasty to the Circumflex were required in '92. The LAD had a 95% narrowing that could not be addressed with angioplasty, but natural bypasses (collaterals) had developed, such that blood flow in the LAD distribution was not severely impaired. Angina recurred in '97. CM received 45 IV EDTA treatments with excellent results; angina resolved and CM was able to resume an active lifestyle.
I first met CM in 3/99; angina was minimal while a rhythm disturbance, intermittent atrial fibrillation, was noted. Chest discomfort became more of an issue in 1/02, and CM's 9:48 stress echo study returned abnormal. I recommended coronary angiography but CM declined (his last angiogram in '92 was complicated by puncture site occlusion and he was needle shy); instead we treated him with four months of Nanobiotic therapy and with this his symptoms improved.
Two years later CM presented with heart failure and pump dysfunction; his ejection fraction (percentage of blood ejected by the heart with each beat - normal is 50%) was only 25%. CM's kidney chemistries were slightly off, and he was now in fixed atrial fibrillation. Medical therapy for CHF was initiated and I pushed CM into an angiogram. The good news here was that the CHF therapy had worked; CM's ejection fraction had increased to 50%, demonstrating abnormal wall motion only over the back wall (1979 heart attack). The bad news was that only two inflow routes to the heart were open, and only by a thread. The Left Main (serves 2/3rds of the heart) had a 90% narrowing. The RCA was occluded, and its vein graft contained a 95% narrowing - everything else was closed. EECP would not work here and I pushed CM into his second bypass surgery. Three new grafts were placed. Kidney function was sluggish following surgery, but otherwise CM's recovery was uneventful. A stress echo study was carried out in 9/04 to clear CM for a cardiac rehab program; CM's resting ejection fraction was 40-45% and the 6:40 stress study looked good.
Chest pain returned in 12/04, just 6 months out from bypass surgery, and CM's stress echo study returned abnormal. CM's resting ejection fraction was 30-35%, and didn't rise with exercise as it should have; CM experienced angina during the study. One or more of CM's grafts has failed. CM wasn't interested in further angiography or surgery, and this time I wasn't going to push him, especially with the mild kidney dysfunction present. CM was treated with 45 hours of EECP, and 100 hours of MME.
CM tolerated both treatments well. His medications were decreased, and with this his kidney chemistries have normalized. CM still experiences chest pain if he pushed himself, but he can walk on the treadmill at 2.8 MPH for 30², and daily activities can be carried out without major difficulty. His resting ejection fraction is up to 40-45%, and following exercise it rises to 50-55%. MME and EECP didn't give CM a new heart, and the 100 hours of MME did not affect CM's atrial fibrillation, but he got better, allowing us to avoid further invasive treatments - we both agree on this.
6-month update - CM continues to well, exercising at a moderate level on a regular basis. I repeated his echo, and saw further improvement as compared to his 2 month post-MME study done in 3/05. I can still see evidence of two prior heart attacks, but overall pump function has improved a little, and the degree of mitral valve regurgitation has decreased some. As in some of our patients with neurological impairments, I'm seeing an ongoing or "late" further improvement in patients with heart disease treated with MME. I'm getting the idea that the stem cell proliferation or reparative processes that we seem to be generating with MME may take some time to manifest themselves as improved heart function and/or better looking non-invasive studies. And really, should I be surprised? It took 9 months for your heart to develop; shouldn't it take an equal amount of time for freshly stimulated cardiac stem cells to "grow up" and do their thing?
12-month update - CM has improved further. He can go longer on his home treadmill, and he hasn't needed a NTG tab in 6 months. Cardiac echo study shows some lessening in the degree of tricuspid regurgitation since 5/05. The pump function gain that CM experienced with MME has been maintained.
Too Far Gone for Bypass in 2000 - BV - 2/05
|
DATE |
EVENT |
| pre '00 | Two prior painless heart attacks |
| 9/00 | Echo: EF 25% with severe mitral regurgitation Angio: LAD and RCA mid-vessel occlusion, Circumflex distal occlusion, Marginal 70%, with an EF of 15% |
| 1/01 | Effort symptoms; resting EF 20-25% with an abnormal 7:00 (modified protocol) stress echo ® 35 hours of EECP |
| 2/01 | Symptoms improved, resting EF 20-25%, with a normal 7:00 stress echo |
| '01 | Five months of Nanobiotic therapy |
| 4/03 | Recurrent angina, addressed with 35 hours of EECP |
| 1/05 | Recurrent symptoms; resting EF 35-45% with mild mitral regurgitation ® 35 hours of EECP and 100 hours of MME - symptoms improved, echo without change |
` BV's heart was too far gone in 2000, but this is a concept that we don't believe in. BV, a previously hypertensive smoker with long-standing diabetes, presented with chest tightness and shortness of breath in the fall of '00. Angiography revealed occlusion of all three major coronary arteries, an ejection fraction of only 15%, and severe mitral regurgitation - BV's heart was shot - too far gone for bypass surgery.
I saw BV for the first time in 12/00. BV's meds were adjusted and a cardiac nutritional program was initiated; the next step was 35 hours of EECP. With these measures BV's symptoms improved such that she could carry out desired activities without major difficulty. BV received 5 months of nanobiotic therapy in late '01, and a repeat course of EECP in 4/03 to address recurrent angina. Symptoms recurred in early '05. At this point BV's ejection fraction was in the 35-45% range, with only mild mitral regurgitation. She received 35 hours of EECP, this time coupled with 100 hours of MME. BV's echo picture did not change (and we really didn't expect it to), while effort related chest tightness and shortness of breath did resolve (our goal). BV was too far gone for bypass surgery in 2000, but with a complementary treatment program, EECP, and now MME, her symptoms are minimal and she can carry out all desired activities without difficulty.
7/06 Update - BV remains improved, and has not required a hospital stay or invasive procedure since completing MME in 1/05. Her cardiac echo is unchanged from 1/05; the gain that BV obtained from MME has been maintained. BV is now going to participate in our study of MME in diabetic neuropathy. This is all pretty good for a 72 year old who six years earlier could not undergo bypass surgery because her heart had been too badly damaged by two prior heart attacks.
EECP and MME for Acute and Chronic Coronary Insufficiency - CD - 6/05
|
DATE |
EVENT |
| '99 | Normal stress echo |
| 12/00 | Abnormal (posterior ischemia) stress echo ® 30 IV EDTA treatments |
| '01 | Normal 15:00 stress echo |
| 8/04 | Abnormal 15:00 (posterior ischemia) stress echo |
| 9/04 | Lead 18 and Mercury 7.8 by challenge testing - Creatinine abnormal at 1.4 |
| 12/04 | Atypical pain - 15:00 stress echo produced acute myocardial infarction |
| 12/04 | Acute EECP ® Chest pain and ST elevation resolved |
| 12/04 | 20 Gauss Magnetico sleep pad with topical DMPS-Glutathione begun |
| 1-2/05 | 35 hours EECP, medical therapy and an extensive nutritional program |
| 3/05 | Lead 9.6 and Mercury 1.2 by challenge testing - Creatinine now normal at 1.1 |
| 6/05 | 100 hours MME to the heart - echo now normal |
CD is a strong willed man. Six years ago he weighed 360 pounds. After a screening stress echo study returned benign, CD began a program of exercise and dietary modification. CD lost 100 pounds. A repeat stress study in '01 returned mildly abnormal. CD underwent 30 IV EDTA treatments, and a follow-up study one year later looked great.
I began working with CD in 8/04. His stress echo study returned mildly abnormal, but he was able to complete 15:00 of treadmill stress. We discussed angiography, but at that time CD was not experiencing any symptoms of coronary insufficiency. We were also worried about his kidneys, and the potential for the X-Ray contrast dye that we use during angiography to damage his kidneys further. CD's creatinine was elevated at 1.4 mg/dl (creatinine reflects the level of kidney function - normal is £ 1.1 mg/dl). A challenge study returned abnormal for Lead and Mercury (see CD's graphics). CD's work involved welding (source of Lead) and his amalgam fillings (2/3rds of tissue Mercury in Americans comes from past and present amalgam fillings) had only recently been removed. A program of risk factor reduction and nutritional therapy was initiated. At that time I didn't think that we needed to be in a hurry, so I began CD on only a moderate dose oral metal detoxification program. In retrospect, not being in a hurry was an error on my part.
CD came in to see me in late 12/04 with upper abdominal discomfort. This didn't sound at all coronary in nature. CD looked good and otherwise he was feeling well. Just to be on the safe side, I repeated his stress echo study. CD and I chatted about our kids during the exam. The chest discomfort in question was present before, during, and after the study; it worsened only slightly with treadmill stress and CD wasn't feeling at all poorly. The post-exercise echo images, however, revealed impaired motion over the back wall of CD's heart, consistent with an at least partial blockage in the artery serving this region, and his EKG demonstrated ST elevation, consistent with a heart attack. I gave CD a sublingual NTG tablet. The NTG had no effect on his pain, nor the appearance of his EKG or echo. Basically, I had precipitated a heart attack in CD (the 2nd time this had happened in my 20 years of practice). I offered to take CD directly to the hospital catheterization laboratory and carry out an emergency angiogram, but he turned me down. He was worried about the potential for kidney damage from the angiogram, and he just wasn't enthusiastic about stent placement or bypass surgery. As stated above, CD is a strong willed man. I'm smart enough to know that I am not going to win arguments with people who can lose 100 pounds in two years, so I went directly to plan B.
In the US, we use EECP to deal with chronic coronary disease and heart failure, but in China EECP is a first line treatment for acute heart attack. We walked CD from the stress room to the EECP room and treated him for three hours. CD's chest pain resolved, as did his abnormal EKG findings (see CD's graphics). CD received two hours of EECP over each of the next five days; a full course of EECP was completed in January of '05.
Obviously we needed to take a more aggressive approach to the factors underlying CD's coronary disease, and we needed to do it post haste. CD began sleeping on a 20 Gauss Magnetic negative field only sleep pad. Every other evening he rubbed 50 drops of transdermal DMPS-Glutathione into his skin, aiming to mobilize and removed from his system Mercury and Lead. 100 hours of MME was carried out in 6/05. On CD's post-MME resting echo study, I could not see any evidence that he had sustained a heart attack (but the amount of damage done in 12/04 was likely minimal, as we had treated him with instantaneous EECP). A repeat challenge study showed that a great deal of Mercury and Lead had been cleared from CD's system (see CD's graphics).
Our plan is for CD to continue his present pharmacologic and nutritional program. He will continue to sleep on the Magnetico pad, and DMPS-Glutathione will be kept on board at a half dose. A stress echo study will be carried out in several months (we are learning that the peak effect of MME is not obvious for several months after MME is stopped). Oh, and by the way, CD's kidney function is now normal; his creatinine is down to 1.1 mg/dl. While we focused on clearing Mercury and Lead from CD's heart, at the same time we must have cleared Mercury and Lead from his kidneys - after all, the Magnetico sleep pad and the topical DMPS-Glutathione that CD applied have access to every cell in your body. I guess it's a good thing that CD is so strong willed. He argued me out of urgent angiography, an approach to his acute heart disease that could easily have damaged his kidneys, and into a program of EECP and negative field magnetic therapy, an approach that got the job done heart-wise, and at the same time improved the function of his kidneys. I like taking care of patients like CD, and I love this approach to medicine. Click CD's symptoms for a description of how CD felt, in his own words, before and after MME.
7/06 Update - CD remains physically active and asymptomatic.
EECP and MME for Refractory symptoms following your 3rd Bypass - DB - 6/05
|
|
EVENT |
| '84 | Bypass surgery with urgent re-do surgery for acute graft failure |
| '96 | Third coronary artery bypass surgery |
| '98 | Normal 7:00 stress cardiolite perfusion study |
| 10/03 | Abnormal 6:00 stress echo study |
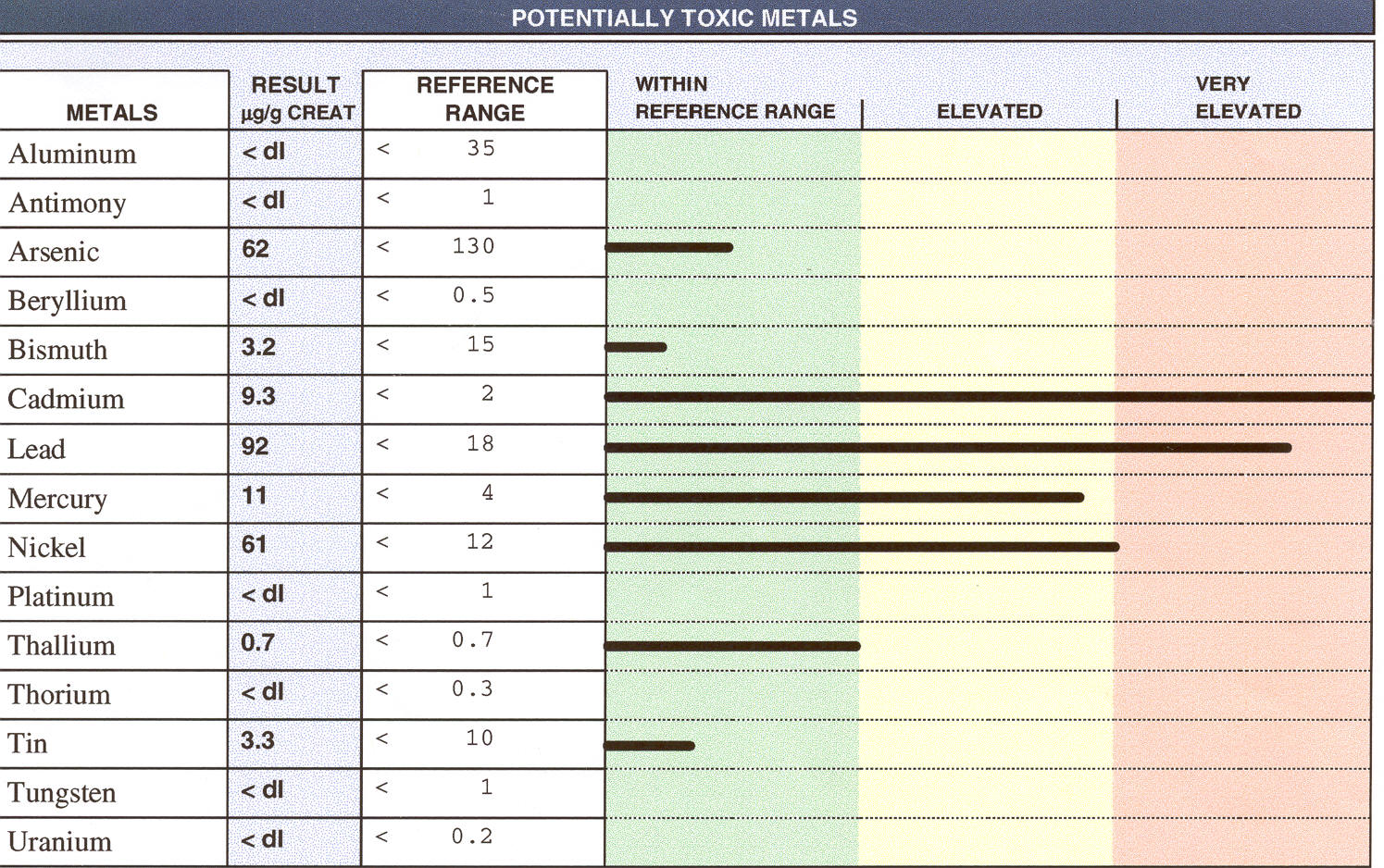
| 10/03 | Cadmium 9.3, Lead 92, Mercury 11, and Nickel 61 by challenge testing |
| 12/04 | Increased symptoms with an abnormal 3:30 stress echo ® Coronary angiography |
| 1/05 | LAD 65%, 1st septal 80%, with an occluded LIMA graft, Circumflex 60% with an open vein graft, Marginal 100% with an occluded vein graft, RCA 100% with a patent RIMA graft, inferior hypokinesis with a normal EF |
| 1-3/05 | EECP with pharmacologic and nutritional treatment as tolerated |
| 3-5/05 | Magnetico sleep pad with topical DMPS-Glutathione |
| 6/05 | 200 hours of MME: Energy level and exercise tolerance increased, BP control improving, as is DB's tolerance to drug and nutritional therapies |
I began working with DB in the fall of "03. Symptoms had recurred, then three years out from her 3rd bypass surgery. DB's BP and lipid values were out of control, and nearly impossible to treat. Multiple BP drugs had been tried; she could tolerate only one - Atenolol. Statin cholesterol lowering agents and Zetia had been prescribed - none were tolerated and CD's LDL was around 200 mg/dl. CD needed help outside the paradigm of more drugs and surgery. It is my observation that patients who just can't tolerate any drugs (and nutritional therapies for that matter) are often metal overloaded. My feeling here is that the enzyme systems involved in drug metabolism and detoxification have been inactivated by the heavy metals. The drugs cannot be broken down and as a result the patient just can't take them - they often can't take anything. I suspected this to be the case with DB. A triple challenge study (low doses of IV EDTA and DMPS alone with oral DMSA and EDTA - followed by a measurement of metals excreted in a 6-hour urine sample) demonstrated spills of Cadmium, Lead, Mercury, and Nickel, supporting my hypothesis. I tried treating DB with an oral preparation containing EDTA and Phosphatidylcholine. DB could tolerate only a low dose (just as she could tolerate only a low dose of anything she could tolerate). With this DB's LDL fell slightly, from 190 to 173 mg/dl.
DB's stress echo study had returned abnormal in 10/03. At that time her symptoms were not marked, and I wasn't enthusiastic about carrying out the angiogram that might lead to her 4th bypass surgery. A repeat stress study carried out in 12/04 looked worse, with an interval decrease in treadmill walking time from 6:00 to 3:30. DB's symptoms were worse too, and thus we proceeded with coronary angiography. This study revealed two open and one closed bypass graft, along with narrowings in the non-bypassed LAD (left anterior descending). Stent placement was not an option here and a 4th surgery risked damage to her two still open grafts. We treated CD with a course of EECP and with this she improved a little. 10 IV EDTA (binds Cadmium, Lead, and Nickel but not Mercury) were administered. Then CD began sleeping on a Magnetico sleep pad, and we switched from IV EDTA to topical DMPS-Glutathione (binds Mercury and to a lesser extent Lead). DB improved further. Her BP became easier to control, and medication intolerance was now less of an issue. After two months of sleep pad/DMPS pre-treatment, DB received 200 hours of MME to her heart. Things are now going DB's way. She will continue to sleep on the Magnetico pad and she will keep up with DMPS based metal detoxification. A stress echo study will be carried out four to six months post-MME, and we will then reassess her treatment plan (please review the following paragraph and then DB's 9/05 update)..
I was trained to think that high cholesterol was the cause of cardiovascular disease. I was trained wrong. Back then we really didn't know what we were dealing with. My thinking is changing. While high cholesterol is clearly an issue, I now feel that heavy metal overload is a more important culprit. It may be that heavy metal overload plays a role not just in the causation of vascular disease, but as a driving force underlying high cholesterol, high blood pressure, and vascular wall inflammation. Heavy metals poison enzyme systems. They can poison the enzymes that carry out reverse cholesterol transport and they can poison the enzymes that make artery dilating substances like Nitric Oxide. Metals poison enzymes and metals poisoned DB. DB's response to MME and metal detoxification supports this new thinking (new to me me anyway). DB's primary problem all along may have been metal overload. We are using EECP, MME, and metal detoxification primarily in patients with end-stage, recurrent, or inoperable patients, patients like DB, but what would have happened had MME and metal detoxification been applied to DB in 1984? Maybe one day, after we prove unequivocally that this approach works (and here we have more work to do), we will be using negative field magnetic therapy/ metal detoxification as a first line therapy - we could call it the DB protocol.
7/05 Update - DB required surgery to address a high-grade carotid artery narrowing; cardiac-wise she did well with the procedure. BP control continues to improve, as does DB's tolerance to prescription medications. In the above paragraph I commented that cholesterol was not the "be all and end all" cause of heart disease as I was taught. In DB's case I might just be right. Her LDL did fall slightly (190 to 173) with an oral chelation program, but in late 8/05, post-MME, and following a total of 5 months of sleep pad/topical DMPS-Glutathione metal chelation, her LDL is down to an all time low of 130 mg/dl - this is in a patient who has never been able to tolerate statin drugs. DB's LDL reduction supports my position that metal overload is playing a role in the progressive, age-related rise in cholesterol that we see in many of our patients. They watch their diet but still their cholesterol keeps rising - because the problem is metal overload - not diet, and not drug deficiency. We will continue to use statin drugs for rapid lipid reduction, but it is only rationale to concomitantly remove toxic metals, and the sleep pad/topical DMPS-Glutathione may be the best approach here.
7/06 Update - DB remains angina free; BP control continues to improve.
Hearing Hoof Beats, Thinking Horses, and Missing the Zebra - KD - 9/04
|
|
EVENT |
| '93 | Lung malignancy ® Resection of 1/2 the right lung |
| '01 | Two vessel bypass surgery |
| 2/04 | ed shortness of breath and an abnormal chemical stress perfusion study ® |
| 2/04 | RCA only 55%, LIMA arterial graft to occluded LAD open, high-grade Left Main - Circumflex narrowing with occlusion of the Circumflex vein graft ® |
| 2/04 | Left Main-Circumflex angioplasty carried out - stent placement not possible |
| 4/04 | No improvement and 4:00 stress echo abnormal ® angiography |
| 4/04 | Left Main-Circ restenosis - further intervention not possible in Toledo |
| 6/04 | Symptoms improved following 35 hours of EECP |
| 9/04 | Symptoms recurred ® 35 hours of EECP and 200 hours of MME - no better |
| 4/05 | Feeling worse ® Left Main-Circumflex narrowing unchanged to slightly better |
| 5/05 | Left Main-Circ narrowing stented in Detroit ® Feels even worse |
| 6/05 | Progressive interstitial lung disease diagnosed - heart wasn't the primary problem |
KD doesn't represent a failure of EECP and MME. The problem here is that I and every other doctor participating in his care missed the diagnosis of progressive interstitial lung disease, and focused instead on his heart, which was not the primary problem.
KD had smoked for years; he had significant emphysema and in '93 lung cancer was diagnosed. Half of KD's right lung was removed; the surgery went well and KD was cured of his cancer. Shortness of breath became an issue in '01. Angiography revealed narrowings in two vessels and two bypass grafts were placed.
Symptoms recurred in 2/04. There was no evidence for recurrent cancer and a chemical stress perfusion study returned abnormal. Recurrent coronary disease, on top of right heart strain due to KD's lung disease, were felt to be the culprits. Heart catheterization was carried out. The blood pressure in KD's right heart was sky high, and his right heart was dilated and dysfunctional (a consequence of chronic lung disease). KD's right coronary artery (RCA) contained only a moderate, 55% narrowing, and the LIMA arterial graft to the LAD was intact, but the vein graft to the Circumflex artery had closed down, and flow to this region was compromised by a 90% narrowing in the Left Main as it gave off the Circumflex. Angioplasty was carried out, opening up the narrowing, but a stent could not be placed (bend in the vessel).
Symptoms recurred two months later. Angiography revealed restenosis at the angioplasty site. Interventional cardiologist in Toledo did not feel that this restenotic narrowing could be safely redilated. KD's lung disease precluded further bypass surgery. KD came to see me and we treated him with 35 hours of EECP, and with this he felt better - for a while.
Shortness of breath recurred in the fall of '04. KD received an additional 35 hours of EECP, along with 200 hours of MME in 2/05. He didn't improve and by 4/05 KD couldn't even walk across the room. He was under the care of a pulmonary physician, who had prescribed bronchodilating agents to optimize the function of the 1 and 1/2 lungs that KD still had left. I was stuck. Single vessel recurrent coronary disease, what KD had, typically responds well to EECP, and KD had received two rounds of EECP plus 200 hours of MME. I began to doubt my thinking. Perhaps EECP hadn't gotten the job done. Perhaps adequate collateral flow had not been generated (we don't necessarily see the collateral vessels on angiography - it is felt that most of the collateral channels generated by EECP are microscopic and not visible to the eye - but we assume they are there). Maybe this single vessel coronary insufficiency was a huge problem, and EECP/MME not an effective answer. I knew that a component of KD's symptoms were due to his emphysema, and a component likely due to his heart. The only thing we could address was his heart, and only with a high-risk catheter-based intervention. No one in Toledo wanted to tackle KD's recurrent coronary narrowing with a catheter based intervention, so I consulted with a colleague in Detroit who specializes in high risk interventional cardiology. KD's angiogram was repeated. The Left Main-Circumflex narrowing actually looked a little better to me, but thinking that coronary insufficiency might be the culprit, and the only culprit we could treat, I sent KD to Detroit for Left Main-Circumflex stent placement. The procedure was carried out without a hitch (my colleague is very good), but KD's symptoms didn't improve; in fact they worsened. His blood oxygen levels began to plummet; his pulmonary status was re-examined and the diagnosis of interstitial lung disease was made. This is a rare, inflammatory condition involving the lungs, progressive and difficult to treat.
KD's coronary disease certainly played a role in his symptoms, but in retrospect we probably treated him adequately with EECP and MME. The high risk Left Main-Circumflex stent procedure was not necessary. KD's problem was that we didn't recognize that something other than emphysema was going on in his lungs. We have a saying in Medicine: "When you hear hoof beats, think horses, not zebras". In other words, look for common things, like emphysema in patients with known emphysema, not exotic diseases like interstitial lung disease. In a man with emphysema and coronary disease we looked for emphysema and coronary disease, and we missed the zebra. I and the other doctors participating in KD's care didn't do anything wrong, but we didn't do anything brilliant either. I am going to learn from this case.
Proactive Magnetic Cardiology - Taking MME to Prevent the Crisis - BP - 4/05
|
|
EVENT |
| 6/98 | Uncomplicated Inferior Wall Heart Attack |
| 7/98 | Abnormal 7:11 stress echo |
| 7-8/98 | 35 hours of EECP |
| 11/98 | Normal 9:30 stress echo - subsequent studies through 5/04 also non-ischemic |
| 5/04 | Normal 7:34 stress echo |
| 4/05 | 92 hours of MME |
| 5/05 | Normal 9:00 stress echo |
The MME patients presented to this point were all in deep trouble. They underwent MME to address active cardiac symptoms. Nearly all of our 1st year cardiac MME patients had previously required surgical or invasive revascularization procedures, and were now troubled by treatment refractory or recurrent/inoperable coronary insufficiency - that's why we treated them with MME. The response to MME of this group of patients has been gratifying, but if MME is helping my patients with far advanced or "too far gone" coronary disease, why not apply it to patients before they get to this point? If MME is effective for the patient in crisis, why not use MME, applied in a low pressure, elective fashion, to help prevent the crisis in the first place?
BP is quite interested in non-pharmacologic, non-surgical approaches to his active health problems, and using the same to prevent future difficulties. 60 hours of MME to his knee all but resolved chronic arthritis pain. 79 hours of MME to his head reduced the severity of chronic tinnitus (ringing in the ears) by 50%. BP has taken a proactive stance regarding his cardiovascular health as well. He watches his diet, takes an extensive program of nutritional supplements, and before we met in '97, BP had undergone 50 IV EDTA chelation treatments. His amalgam fillings had been removed, but BP had not received any medical Mercury detoxification therapy.
BP sustained an uncomplicated heart attack involving the back wall of his heart in mid-'98. A stress echo study one month later returned abnormal - a small scar was seen, along with additional heart muscle at risk for further damage. The amount of muscle at risk did not appear to be excessive, and BP was not feeling poorly, so we elected to skip coronary angiography and instead treated BP with 35 hours of EECP. This worked well. Post-EECP BP walked 2:19 longer on the treadmill and his echo study showed no additional heart muscle at risk - EECP had done its job. BP kept up with risk factor reduction and his extensive nutritional regimen, and subsequent stress echo studies have all looked good. BP's 5/04 study also returned non-ischemic, remarkable only for a small scar from his 6/98 heart attack, but his treadmill time was down to 7:34 (but BP was also 6 years older).
I do not have BP on any cardioactive medications, nor have I recommended that he undergo coronary angiography, as his current situation is stable and non-threatening. BP would like his situation to remain stable and non-threatening, so he chose to undergo 92 hours of MME to his heart. PB had been sleeping on a Magnetico negative field only sleep pad, and he was pre-treated with oral DMSA, which was continued during MME.
Pre-MME BP was feeling well, without angina, but post-MME BP is feeling better, lighter on his feet, with more energy - "this is the best I have felt in years". We repeated BP's stress echo study, more out of curiosity than anything else. Treadmill time had increased from 7:34 in 5/04 to 9:00 on his 5/05 post-MME study. I could still see evidence of BP's remote heart attack, and as expected, there were no findings to suggest that additional heart muscle was at risk. BP had been doing well, but post-MME he is doing better. Our hypothesis is that MME increases the generation and utilization of ATP energy within the heart, and that this energy is used not just to improve cardiac performance, but also to repair any abnormalities present within the ultrastructure of the cardiac cells. We think that MME drives toxic metals out of the heart, toxic metals that inactivate the enzyme systems that govern cellular physiology. We feel that by these means, MME can take a good heart, like BP's, and make it better. Maybe BP's heart is no longer 6 years older - it doesn't act like a 6-year-older heart. We predict that the application of MME to patients like BP will decrease their risk of future crisis, future episodes of coronary insufficiency or heart failure. Time will tell if we are right or not. In the meantime, BP is feeling better, my goal as his physician.
7/06 Update - BP remains asymptomatic, active, and interested in life. He feel in love again (with his magnetically treated heart) with a beautiful woman and they plan on living happily ever after.
MME and EECP for Refractory Angina in a 92 year old Golf Enthusiast - RM - 7/05
|
|
EVENT |
| '89 | Uncomplicated Heart Attack followed by balloon angioplasty |
| 5/05 | Second heart attack - LAD 95%, patent 1st and 90% narrowed 2nd diagonal; Circ. patent with 99% 1st and 80% 2nd marginal branch narrowings; RCA 100% with moderate to severe mitral regurgitation and an ejection fraction of 30% |
| 6/05 | Persistent angina despite maximal medical therapy - EF 20-25% by echo |
| 7-8/05 | Bioenergetic nutritional support, 45 hours EECP, and 250 hours of MME |
| 9/05 | Angina fully resolved at a modest activity level - EF 25-30% by echo |
| ® | Sleep pad, oral metal detoxification, and ongoing drug and nutritional therapy |
RM enjoys a good game of golf - but he had a bad day on the course in May '05. RM sustained an uncomplicated heart attack in 1989. Single vessel balloon angioplasty was required, but since then, with ongoing medical therapy, RM has felt well, able to play 9 holes of slow golf - not bad for a coronary patient in his 90s. We had a lousy Spring '05 in Toledo - Winter didn't want to end. RM couldn't get back on the links until early May. That morning he played a game of pool, without difficulty. On the course he didn't feel as well. He walked the 1st six holes, but experienced shortness of breath with effort. RM used a cart for the remaining three holes, but his breathing didn't get any better, and he began to experience heart pain (for RM an aching sensation in his upper back). An ambulance was summoned. RM was in the midst of a heat attack. RM was stabilized an angiography was carried out the following day. The RCA (right coronary artery - serves the back wall of the heart) was occluded. The LAD (left anterior descending - serves the front wall) had a 95% narrowing, and its 2nd diagonal branch a 90% blockage. Both branches of the Circumflex (serves the side wall of the heart) had critical obstructions. RM's ejection fraction (percentage of blood volume ejected with each beat - normal is 50%) was only 30%, and his mitral valve was not functioning normally, allowing regurgitation of blood back from the left heart into the lungs.
There were no narrowings in RM's coronary vasculature suitable for balloon angioplasty or stent placement. Bypass surgery wasn't possible, not because of RM's age, but due to the heavy calcification of RM's vessels - the heart surgeons were worried that they wouldn't be able to sew in a graft. Medical therapy was advanced and RM was discharged home - but he couldn't do anything. RM continued to experience angina with minimal activity, and occasionally at rest. When I saw RM in late 6/05, he was experiencing angina; his ejection fraction was in the 20-25% range, while the degree of mitral regurgitation had lessened. A program of cardiac nutritional support was initiated (Carnitine, Co-Enzyme Q10, Antioxidants, Fish Oil, etc.) RM's coronary system was essentially too far gone for EECP - the only vessels from which collateral flow could be generated were the Circumflex proper and the proximal LAD) - but RM had no other options - so we treated him with EECP combined with MME (after all, the reason we brought MME to town was to help patients too far gone for EECP).
RM received 45 hours of EECP and 250 hours of MME. He tolerated both treatments well (his BP fell a little - arteries becoming more elastic - we decreased his drugs a little to compensate). As of 9/1, RM is angina free. He can be seen walking briskly in the halls of our office. Swinging a golf club in his back yard will make RM short of breath, but he can carry out activities of daily living without major difficulty. Medical and nutritional therapy will be continued. RM will sleep on a negative field only pad, and he will take an oral metal binding agent. RM's cholesterol is well controlled medically, but our work up revealed an off the chart Lp(a) of 101 mg/dl, which we will take aim at.
I'm not sure if RM will improve to the point where he can again take aim at a golf ball again, but with EECP/MME, his angina has resolved and his quality of life has certainly improved - not bad in a 92 year old with advanced pump dysfunction and an inoperable coronary picture.
7/06 Update - RM did get back on the golf course last fall. He felt well, so well in fact that he decided to get up on a step ladder to hang Christmas ornaments. RM slipped and fell, and sustained a complicated fracture of his left shoulder. Surgical fixation was not possible. RM had to stop exercising, and with this his chest discomfort returned. We treated RM with a booster course of EECP, concomitantly with 100 hours of MME to his shoulder. This program worked; RM can't raise his arm above the level of his shoulder, but he can swing a gold club, which is what he is interested in. RM's angina resolved, and his echo picture is stable, with an ejection fraction in the 30-35% range.
Bringing back Memories - MME and EECP for the Heart and Mind - SP - 8/05
|
|
EVENT |
| 7/94 | Bypass surgery - LIMA to LAD and SVG to RCA; Circ intact and not bypassed |
| 1/95 | Recurrent symptoms - SVG to narrowed RCA had closed; LIMA to LAD open with a retrograde 95% narrowing, isolating the proximal LAD distribution |
| '98 | 35 hours EECP - symptoms resolved with a now normal 7:00 stress echo |
| ® '02 | Two EECP boosters, drug and nutritional therapy - no hospitalizations |
| 1/03 | Angina - RCA now with two 90% distal lesions - otherwise no change from '95 - Circ. normal, LIMA to LAD intact, with a retrograde 95% narrowing |
| 1/03 | One RCA narrowing stented and one balloon dilated (stent not possible) |
| 1/05 | Angina - 70% narrowing at the 1/03 balloon angioplasty site |
| 8-9/05 | 35 hours of EECP and 200 hours of MME ® Improved cardiac status & memory |
| ® | Topical DMPS-Glutathione |
Standard drug and surgical approaches to heart disease benefit the heart, but may produce side-effects, compromising other organ systems. EECP, MME, and the nutritional and detoxification measures that we employ benefit the heart, do not have side effects, and they benefit every other organ system in the body. If you don't believe me, just ask SP where he hid his prized baseball when he was 7 years old.
SP had been under my care for a decade. Using a mixture of drug and nutritional approaches and several courses of EECP, I haven't fully resolved his symptoms, but under my care the quality of SP's life has been good, and he hasn't required a single trip to the emergency room. SP underwent angiography for the first time in '91. A 40-50% LAD narrowing was noted, while the remaining vessels were clear. His doctors did not put SP on a risk factor reduction program, and SP's narrowings progressed. Symptoms developed in '94. The LAD now had a 95% narrowing, and the RCA had developed a 55% constriction. A LIMA (Left Internal Mammary Artery) graft was placed to the LAD and a SVG (Saphenous Vein Graft) to the RCA. One year later SP returned with more trouble. The vein graft had occluded. Further surgery made little sense and the RCA narrowing was not tight enough to warrant balloon angioplasty. We began SP on a risk factor reduction program and tided him over with medical therapy, and when EECP became available in Toledo, we treated him. Between '98 and '02, we kept this program up, and SP did well. In early '03, however, SP's symptoms recurred. Angiography revealed disease progression in the RCA, as it divided into two branch vessels. One branch was balloon dilated and stented; the second was balloon dilated but the vessel was too small for stent placement. SP did well for two years, but in early '05 his symptoms recurred, and we found a 70% narrowing at the balloon dilatation site - everything else was stable. The interventional cardiologist working with us did not feel that repeat angioplasty would work. He did feel that a new, low profile, medicated stent might be appropriate for SP's 70% narrowing, but this particular device was not expected to be released for another six months.
So what more could we do? My best efforts had kept SP out of trouble for a decade, but no longer were getting the job done, and the new stent wouldn't be available for 6 months. Well, with the addition of MME to the program, my best efforts were now a little better. SP received 35 hours of EECP, coupled with 200 hours of MME, in 50 four hour sessions. With each MME session, SP received 500 mg of DMSA, an oral Mercury, Lead, and Cadmium binding agent. While our focus is on SP's heart, the DMSA will remove metals from every cell in SP's body, and SP's brain will receive a little of the MME effect.
I last saw SP as he was finishing EECP; at that point he had also completed 168 hours of MME. His cardiac symptoms had improved. Chest tightness had fully resolved. Shortness of breath was still an issue with greater than usual activity, but SP could carry our yard work (sawing tree limbs) without major difficulty, and we were able to drop Nifedipine (a cardiac drug) from SP's program. This we expected, but what is really interesting about SP's response to EECP/MME is the improvement that occurred elsewhere is SP's body (see SP's symptoms). Early on SP would experience slight disorientation following his MME treatments. This disorientation resolved, giving way to improved memory. SP recounted to me a number of childhood and adult memories, memories that he had lost. SP is 81, and when he was growing up, real baseballs were a prized possession. Most of the time you played baseball with a ball of yarn, tied down tightly by layers of wound string, that your Mom made for you. As a kid, SP was good at checkers. One night he beat his Dad's best friend, who was so impressed with SP that he gave SP a real calf hide baseball. SP and his friends shared the ball during the day, but each night SP made sure the ball returned home with him - it was his prized possession. SP was worried that one of the neighborhood kids might sneak into his room and take the ball. SP established a secret hiding place, in a cherry tree in his backyard. Each night he would sneak out of the house and stash the ball in the tree; each morning he would retrieve it - this became part of his childhood. This was an important memory, like your childhood dog, your first little league hit, or your first kiss in high school, but this memory got lost. SP hadn't had these recollections, these thoughts about childhood baseball, checkers, or his secret hiding place, for years, but these childhood memories came rushing back following MME. I think the transient disorientation that SP experienced early on with MME was a detoxification reaction - toxic metals exiting the nervous system and neural pathways opening back up. When we treat your heart with MME, there is a scatter of magnetic energy to your brain, and the DMSA works in the brain, just as it does in your heart.
Ideally, SP would keep up with negative field magnetic therapy, by sleeping on a Magnetico sleep pad, but cost here is a constraint. What SP will do is to apply topical DMPS-Glutathione (a fairly low cost metal binder) every other evening, to keep up this process of removing toxic metals from his heart, his brain, and elsewhere in his body. SP's interventional cardiologist (a close colleague of mine) may have lost a difficult stent case (and he will be pleased with the situation) while I will look forward to hearing more stories of SP's youth.
Two for One - MME for the Heart and the Lungs - JI - 9/05
|
|
EVENT |
| '95 | Four vessel bypass surgery, with a 6 month Staph wound infection |
| '03 | Two grafts open and two grafts closed - multiple stents placed in the RCA |
| '04 | Shortness of breath from emphysema: FEV-1 only 48% predicted |
| 6/05 | Echo - left atrial enlargement with reduced left ventricular compliance (stiff heart from ATP depletion) |
| 8/05 | Effort angina - Adenosine perfusion study with LAD ischemia and heart dilatation |
| 9/05 | 252 hours MME - split between right and left lungs (there covering the heart) ® ♥ Angina improved with a non-ischemic 9:00 stress echo study ♥ Echo with normal left atrial size and normal ventricular compliance |
| ® | Sleep pad, TD·DMPS-Glutathione, oral PPC, & prior drug and nutritional regimen |
| 10/05 | Pulmonary function studies improved - FEV1 increased by 15% |
JI smoked for 30 years, but he quit 30 years ago. This 75 year-old man has always been active; he is not diabetic, and his BP and cholesterol have been under good control. JI did what he was supposed to do. JI's doctor told JI that he was "the picture of good health" - that is, until '03 when a foot problem led to a vascular evaluation that lead to surgical revascularization of a clogged right carotid artery. Shortness of breath in '04 led to a pulmonary evaluation. IJ's FEV-1, the amount of air that he could exhale in one second, was only 48% of normal, consistent with emphysema. Four vessel coronary bypass surgery was required in '05 - a procedure unfortunately complicated by a Staph sternal wound infection that took 6 months to heal. Leg pain with walking led to placement of a stent in IJ's right Iliac artery; the Plavix anticoagulation necessary post-stent placement led to bladder hemorrhage, requiring cautery.
JI has not taken this sitting down (except before Iliac artery stent placement when he couldn't walk). He has seen a number of medical specialist and is on a number of appropriate medications. JI has also sought counsel and treatment from a number of complementary physicians, including several leaders in the field, practitioners who I respect a great deal. JI has received a number of IV treatments with EDTA (removes Lead and Cadmium), DMPS (removes Mercury) and Polyenylphosphatidylcholine (promotes reverse cholesterol transport and reduces plaque in humans - extensively studied in Europe), and he is on a number of nutritional supplements. Even though JI has undergone IV chelation therapy, challenge studies continue to bring out Nickel, Mercury, and Tungsten.
Effort related chest discomfort became an issue in mid-'05. A cardiac echo described left atrial enlargement and reduced left ventricular compliance - here the heart muscle is not relaxing appropriately, due to deficient regeneration of ATP energy stores, such that the blood pressure within the heart rises, leading to left atrial enlargement and shortness of breath as the high pressure is transmitted back to the lungs, a problem that IL's lungs, already compromised by emphysema (and possibly still Cadmium overload) from prior smoking. An Adenosine chemical stress study revealed ischemia (compromised blood flow) in the distribution of the left Anterior Descending coronary artery (serves the front wall of the heart), and transient cardiac dilatation, suggesting that a significant amount of heart muscle was underserved and at risk.
So what was JI to do? He was already on three anti-ischemic, anti-anginal drugs. Angiography would not likely reveal a narrowing that could be easily addressed with stent placement. His first bypass surgery was complicated by a 6 month wound infection, and his surgical risk with a second bypass procedure, at age 75 with IJ's multiple health problems, would be quite high. EECP was a theoretical possibility, but the presence of poor blood flow to IJ's lower extremities would compromise the efficacy of this approach.
What JI did was to call Dr. Bonlie, who advised JI to consult with me, as my background and area of expertise is in the treatment of patients with inoperable coronary disease (why we got the MME machines in the first place). I spoke with JI and his wife over the phone on several occasions, reviewed his medical records, and worked up a treatment plan. JI then flew to Toledo and received 252 hours of MME over 21 nights, 126 hours to the right lung, and 126 hours to the left lung field and heart.
As we are learning, the peak effects of a course of MME may not be apparent for some time (with regards to improving wall motion in patients with prior heart attack, perhaps not for one year), but JI improved during his stay in Toledo. Effort angina has lessened. We carried out a stress study, this one with treadmill exercise as opposed to chemical stress. The study was done with JI on most of his prior medications (as he would go home on these agents), and the Beta-blocker prevented IJ's heart rate from reaching the target, but JI was able to complete 9:00 of treadmill exercise (quite good for a 75 year-old, with or without coronary artery disease) and no abnormalities were brought out - in other words, JI appeared to be protected at a vigorous exercise level. I felt that JI's left atrium was normal in size, and the echo findings of reduced left ventricular compliance, consistent with deficient cardiac ATP energy regeneration, had resolved. This is certainly a positive, but it shouldn't surprise us, as we know from the literature that static magnetic fields stimulate the generation and utilization of intracellular ATP energy packets.
JI will sleep on a negative-field only magnetic sleep pad, and for ongoing metal detoxification every other evening he will apply topical DMPS-Glutathione. JI will take Polyenylphosphatidylcholine (PPC) in oral form, to promote reverse cholesterol transport, and he will keep up with his prior regimen of drugs and nutritionals. Pulmonary function testing will be carried out later this fall, and I recommended a follow-up DMPS challenge study be done in 4-6 months, to monitor IJ's heavy metal status and to guide further therapeutic decision making.
10/05 Update: Pulmonary function testing was carried out in 10/05, and compared against JI's last pulmonary exam on April '04. The results are presented below in chart and graphic form.
| Measure | Explanation | 4/04 | 10/05 | % change |
| Forced Vital Capacity - FVC - (L) | Volume of air you can exhale | 2.4 | 2.9 | 21% |
| Forced Expiratory Volume - 1 | Volume exhaled in 1 sec. | 1.02 | 1.17 | 15% |
| Vital Capacity - SVC | Total lung volume in liters | 2.4 | 3.4 | 42% |
| Inspiratory Capacity - IC | Volume you can inhale | 1.6 | 2.4 | 45% |
| DLCO - Diffusing Capacity | Rate gas can cross the lungs | 8.8 | 14 | 59% |
Forced Vital Capacity represents the volume of air that you can exhale in one
breath while the FEV1 measures the volume you can exhale in one minute.
Patients with asthma and emphysema cannot exhale fully and rapidly; The
improvement here reflects a reduction in airway constriction or bronchospasm.
SVC refers to total lung volume and IC to the volume of air you can inhale;
both increased. DLCO, or Diffusing Capacity, represents how rapidly a gas can
cross the lung surface - in ST the DLCO rose by 59%, from 37% of normal to 59%
of what is expected in an aged matched man with normal lung function.
These studies demonstrate that not only did ST's heart function improve, so
did his lung function - and why not? The lung can be detoxified and the
lung has stem cells.
EECP and MME following bypass and four rounds of stenting - ST - 9/05
|
|
EVENT |
| 5/00 | Three conduit, four vessel bypass surgery; prior inferior wall heart attack |
| 7/02 | Angina - Non-bypassed Circumflex stented |
| 12/02 | Angina - Stent narrowed ® Redilated with Brachytherapy (radioactive stent) . New narrowing in the marginal branch of the Circumflex ® Stent placed |
| 4/05 | Angina - 90% narrowing in LIMA graft to LAD stented Two vein grafts intact - graft to 2nd diagonal closed 70% renarrowing in marginal stent |
| 4/05 | Benign 10:21 stress echo post-stent placement |
| 7/05 | Unstable angina - New 80% narrowing in LIMA stented, marginal now closed, both vein grafts still open, stent placed in right coronary artery |
| 8/05 | Recurrent angina with rest pain on maximal medical therapy |
| 9/05 | 35 hours EECP and 300 hours of MME ♥ Back to farm work with minimal angina ♥ Echo - inferior contraction abnormality no longer regionally expanded; EF normal ♥ Prinivil and Imdur discontinued |
| ® | Sleep pad, DMSA, and prior drug and nutritional regimen |
| 11/05 | Normal 11:00 stress echo study |
ST has been a model patient. He quit smoking years ago, and remains fit and active running a dairy farm. With diet and medical therapy ST's BP, sugar, and lipid values have been under great control. ST's Lp(a) is elevated, at 47 mg/dl, and this has not been addressed, because it wasn't measured before we bean working together in late 4/05. Lp(a), sometimes called the "ugly cholesterol" serves as a repair particle, and unfortunately it tries to repair the damage done to the vessel lining following angioplasty or stent placement - Lp(a) is strongly associated with restenosis, but there are no drugs that address it (only nutritional agents like vitamin C, fish oil, lysine, and proline), so it is typically ignored by drug oriented physicians. Many of the patients who see us with recurrent coronary disease have sky high Lp(a) levels.
ST had sustained a non-extensive but locally severe heart attack to the inferior or back wall of his heart - on echo you could see this region bulge out. Three grafts were placed to four vessels in 5/00. The non-bypassed Circumflex required stent placement in 7/02. This renarrowed within 5 months (the Lp(a) effect), requiring re-dilation and placement of a radioactive stent (brachytherapy). The marginal branch of the Circumflex had also developed a narrowing and was stented.
ST experienced recurrent symptoms 2 & 1/2 years later. The radioactive stent looked good, while the stent in the marginal vessel had developed a 70% blockage, but the problem now was a 90% narrowing within the LIMA (Left Internal Mammary Artery graft) to the LAD; this 90% narrowing was stented. The vein graft to the right coronary artery was intact; the vein graft to the 1st diagonal branch of the LAD was open, but then was closed before it reached it's 2nd target, the 2nd diagonal branch of the LAD. ST's interventional cardiologist wanted to hold off on re-dilating the marginal stent unless symptoms returned.
ST and I began working together at that point. As stated above, ST was on a comprehensive drug regimen, including a statin and Plavix, and his BP, glucose, and standard lipids looked great, but we found an elevated Lp(a), a low free Testosterone level, and a body burden of Lead as additional causes of coronary disease that we could attack. A 10:21 stress echo study looked good, consistent with open stent sites.
ST required a course of Prednisone to address a hearing issue in 8/05. Whether Prednisone was the culprit (it can raise blood sugar in diabetics) or coincidental we will never know, but one week later ST's coronary symptoms recurred. Angiography demonstrated a new 80% narrowing at the lip of the LIMA graft stent, which was addressed with a new stent. The marginal stent, which contained a 70% narrowing in 4/05, was now closed, and could not be dilated. While the vein graft to the RCA was open, a narrowing in the native RCA did compromise blood flow to the back wall of ST's heart and was stented.
Following this round of stenting (round 4) ST didn't bounce back well. In fact, chest pain recurred within 4 weeks, with occasional episodes of rest pain. ST did not want to undergo round 5, and there was no room to advance his medications further, so we treated him with EECP and MME. ST did great. His angina steadily improved, and we had to back off on ST's drug therapy as his BP fell a little during MME (healthy arteries dilate normally and don't need drugs). An echo done following 300 hours of MME demonstrated impaired function over the back wall of ST"s heart, consistent with his prior heart attack, but the region no longer bulged out. Function elsewhere was brisk an ST's ejection fraction was normal (I had rated it at 45% in 4/05).
ST is back at work, running his farm, and now experiences angina only when working hard under stress (see ST's MME evaluation). He is sleeping on a 20 Gauss sleep pad, taking DMSA to clear Lead from his system, and ST is keeping up with a comprehensive nutritional program, including agents on board to deal with Lp(a). A stress echo study will be carried out in the late fall of '05, and we will repeat ST's resting echo at the 1 year point (we are seeing late improvement in wall motion post-MME - we hypothesize that it takes 9-12 months for stem cells stimulated during MME to "grow up" into functioning heart cells). The overall goal, of course, is to keep ST away from round 5.
1/06 Update - ST underwent stress echo testing in 11/05. The resting echo demonstrated a mild impairment in wall motion over the inferior wall, related to ST's 5/00 heart attack. ST exercised for 11:00, without chest pain, EKG or echo findings of coronary insufficiency. This was a totally normal stress echo study. ST continues to do well, running his farm without difficulty.
7/06 Update - Angina recurred in 4/06; angiography revealed restenosis of the LAD stent site. The RCA stent site looked good. There was no evidence for disease progression in ST's native vessels and overall pump function looked better than in 7/05. This is the second episode of LAD stent restenosis. It just might not be possible for any therapy to prevent recurrent restenosis with this much hardware in the LAD. The good news is that the other vessels and stent sites had not progressed. ST is again angina free; a 10:52 stress echo study carried out in 7/06 looked good.
MME in Inoperable Ischemic Cardiomyopathy - MJ - 10/05
|
|
EVENT |
| 8/03 | CHF with chest tightness; EF 20-25% by echo ® Drug & nutritional therapy begun |
| 11/03 | Catheterization - RCA 100% and mid-LAD 95% with absent wall motion in their distribution; Circumflex clear, EF 20% with PCW 22 and PA 69/36 mmHg |
| 12/03 | 35 hours EECP ® Chest tightness resolved and echo EF now 30-35% |
| 4/05 | Recurrent symptoms - EECP not
possible (insurance issue) Echo - EF 30-35% with 1-2 plus mitral regurgitation Catheterization - PCW 16 and PA 38/20 - arteries not restudied |
| 10/05 |
300 hours MME, preceded by sleep pad/ DMSA therapy over two months ♥ Effort shortness of breath and abdominal bloating improved; wgt. down 5 lbs. ♥ Echo - EF 30-40% with trivial mitral regurgitation |
MJ presented in the summer of '03 with pronounced biventricular heart failure. Lower extremity swelling was marked. Just walking across the room left MJ short of breath. Diuretic therapy was initiated and cleared off the edema fluid. MJ's workup revealed pump dysfunction on the basis of at least two prior painless heart attacks. Catheterization demonstrated occlusion of the Right Coronary Artery (RCA) and akinesis (lack of thickening and inward motion) over the back wall of MJ's heart, the region served by the RCA. At it's mid-point, the Left Anterior Descending (LAD) contained a 95% narrowing, with severely impaired function in the muscle that it served. MJ's third artery, the Circumflex, was free of disease. The filling pressure of MJ's left heart, the PCW, the pressure experienced by his lungs, was elevated at 22 mmHg (normal is < 10), and the pressure experienced by his right heart, the PA or pulmonary artery pressure, was elevated at 69/16 (normal is 25/10 mmHg).
MJ's heart was too far gone for bypass surgery. Standard drug therapy for coronary insufficiency and CHF was continued, but MJ could tolerate only a few of these agents, and these only at low doses. Standard nutritional therapy for coronary insufficiency and CHF, well tolerated by MJ, was continued, and he received 45 hours of EECP. MJ responded with a resolution of chest tightness. He could now walk one mile slowly without significant breathing difficulty. We found MJ to be iron overloaded (Ferritin 584 - ideal is 100 or below) and began to address this problem with iron binding therapy. MJ was maintained on as much drug and nutritional therapy as he could tolerate.
Things went well until April '05. For cost reasons, MJ had to go of iron binding therapy. Shortness of breath with effort recurred. Cardiac echo study revealed an ejection fraction of 30-35%, with mild to moderate mitral valve regurgitation. I repeated MJ's right heart catheterization and found his filling pressures to be improved from 11/03, but still on the high side - MJ's diuretic therapy was advanced. I did not repeat MJ's coronary study as I did not think that he would be a candidate for bypass surgery. MJ now had a different insurer - the only one that will not cover EECP.
In August '05 MJ began sleeping on a 20 Gauss Magnetico negative field only sleep pad while taking oral DMSA at bedtime. Two months later a 300 hour program of MME was carried out. MJ was just finishing MME at the time of this writing - he is experiencing less shortness of breath with effort and abdominal bloating has improved. His weight is down by 5 lbs. MJ's ejection fraction has increased from 30-35% to 30-40%, wall motion over the non-damaged proximal anterior wall is now brisk, and mitral regurgitation is now only negligible. We expect to see a further improvement in pump function over time (We feel that we are stimulating myocardial stem cells to proliferate and migrate, so we need to give the stem cells time to "grow up"). MJ will keep up with DMSA therapy, and I will monitor his course.
7/06 Update - MJ continues to do well. A program of Bioresonance Therapy was carried out over the first 6 months of '06, and following this MJ's primary care physician was able to discontinue MJ's diuretic, Zaroxylyn. Cardiac echo study in 6/06 showed no change from MJ's post-MME study of 10/05.
MME for Coronary Disease and/or Cardiomyopathy - CE - 12/06
|
|
EVENT |
| 9/06 | Fatigue during runs with ST depression on a 13:00 stress EKG study |
| 10/06 | 10 EDTA, 10 HBO, and 20 EECP sessions |
| 12/03 | 35 hours EECP ® Chest tightness resolved and echo EF now 30-35% |
| 10/06 | 14:33 stress echo - fixed inferior and reversible anterior contraction abnormalities |
|
10
® 12/06 |
DeToxMax, Zeolite, and sleep pad/DMSA therapy 200 hours MME, preceded by sleep pad/ DMSA therapy over two months |
| 12/06 | 15:00 stress echo - foxed inferior abnormality - anterior wall now normal |
I couldn't tell whether CE's symptoms were due to coronary disease, long
standing hypertension, cardiomyopathy, or all three - but this may not be an
issue as MME based detoxification should be able to help with all three.
CE has been on medical therapy for hypertension for at least a decade.
CE was also on a comprehensive nutritional program, he exercised on a regular
basis, and CE felt great.
CE felt great until until mid '06, when he began to experience fatigue while running. Cutting back to a slow job helped for awhile, but then CE had to slow down even more. Something was wrong - CE saw his physician who initiated a cardiovascular workup. CE's cardiac echo demonstrated diastolic dysfunction, a "stiff heart", probably on the basis of hypertension. CE walked 12:59 on the treadmill - PVCs, extra beats from the ventricles, the pumping chambers, were brought out, along with ST segment depression, worrisome for coronary insufficiency. Angiography was recommended but CE did not feel comfortable with invasive intervention - after all his exercise capacity remained well preserved, and he was experiencing symptoms only with strenuous effort.
CE obtained a second opinion at the Whitaker Clinic in California. There CE received 10 IV EDTA treatments, 10 sessions of hyperbaric oxygen therapy (HBO), and a half course of EECP. CE splits his time between Arizona and NW Ohio - it was time to return to Toledo and the plan was for CE to complete his program of EECP here.
First I repeated CE's stress study, this time with concomitant echo imaging. CE walked for 14:33. ST depression was brought out. The inferior wall of CE's left ventricle looked sluggish at rest and following treadmill stress, while dysfunction of the anterior wall developed following treadmill exercise. This pattern could reflect a prior inferior wall heart attack with the anterior wall at risk due to a narrowing in its blood supply, or this pattern could reflect cardiomyopathy, a generalized weakness of the heart muscle, perhaps aggravated by the effects of long standing hypertension. Angiography would settle the issue but CE wanted to remain non-invasive (and with a 14:33 treadmill time I did not need to push him towards an invasive approach).
My challenge was to construct a treatment program that could address all three of CE's potential cardiac problems. CE continued his prior nutritional program and we added DeToxMax (EDTA and dilinolenylphosphatidylcholine in a well absorbed oral format), aiming to unpoison and then stimulate the enzymes of reverse cholesterol transport. CE began a program of oral Zeolite and DMSA, before retiring for the night on a 20 Gauss negative field sleep pad. CE then received 200 hours of MME, completing treatment just before the holidays in 12/06.
CE's stress echo was then repeated - treadmill time was 15:00 - abnormal ST depression was not brought out - again I could see a fixed inferior wall contraction abnormality but the effort induced anterior abnormality was not longer present. My current thinking is that CE sustained an inferior wall heart attack at some point, and that our treatments have improved blood flow in the vessels serving his anterior wall. My hunch is that, in six to nine months, we will see an improvement in inferior wall function, as stem cells that we stimulated with MME have a chance to "grow up" and function (this is the time course that I have seen in others and is consistent with our theory as to how MME regenerates damaged organs). CE is also going to get involved in our Asyra based homeopathic treatment program and is planning on undergoing a series of LED (Laser Energetic Detoxification) treatments. His stress echo study will be repeated in the future.
MME to help a Dilated Cardiomyopathy patient get back on his bike - BH - 9/04
|
DATE |
EVENT |
| 3/01 | Gradual onset of fatigue and shortness of breath with effort |
| 7/01 | Cardiac echo - Ejection fraction (EF) 20% with severe mitral regurgitation EKG - Atrial fibrillation |
| 9/04 | Symptoms - Short of breath with mild activity EKG - Atrial fibrillation Echo - EF 15-25%, severe mitral (8 cm2) and moderately severe (9cm2) tricuspid regurgitation with a Pulmonary Artery (PA) systolic pressure of 60 mmHg |
| 9/04 | 138 hours of MME |
| 10/04 | Symptoms - Fatigue and shortness of breath improved; able to ride his bike EKG - Atrial fibrillation Echo - EF 25-30%, less mitral (5 cm2) and nearly resolved tricuspid regurgitation with a PA systolic pressure of 40 mmHg |
| 9/05 | Feeling even better - riding his bike up and down the hills of Va. |
BH and his wife have done a lot for me. They've done a lot to protect health care freedom for physicians and patients. People like BH and his wife have made it possible for people like me to treat people like you with MME and other innovative therapies. Now it was my turn to help BH.
BH began to experience symptoms of heart failure in the spring of 2001. Physical activity that used to be easy was now hard. Ankle swelling developed, along with fatigue. BH could no longer do the things he liked to do. Medical evaluation led to the diagnosis of heart failure (CHF for congestive heart failure) due to dilated cardiomyopathy (a generalized weakness of the heart muscle, not on the basis of coronary artery disease).
BH was surprised - he'd done all the right things and never expected to get sick. BH ate right, exercised on a regular basis, took a well-thought-out program of nutritional supplements, and received regular IV EDTA chelation treatments (264 in all). EDTA removes toxic heavy metals (Lead, Cadmium, and Arsenic - but not Mercury) from your body. Still, BH was in heart failure; the cells of his heart were sick. He wasn't born with cardiomyopathy, so some environmental process had damaged his heart, and he was in trouble.
Conventional pharmacologic treatments were tried, and were not tolerated well. BH wound up on a diuretic (water pill), to help clear retained fluid, and digoxin (to control his heart rate), which was rapid and irregular due to an arrhythmia, atrial fibrillation. BH sought the counsel of the leading minds in the field of nutritional medicine, and constructed for himself an incredibly comprehensive nutritional program for CHF control. BH's program has helped a lot of other people, and it kept BH out of the hospital, but he still wasn't well. When I saw BH in early 9/04, he was experiencing shortness of breath with modest effort, and his cardiac echo study demonstrated an ejection fraction in the 15-25% range (percentage of blood ejected with each beat - normal is 55%), severe leakage of the mitral and tricuspid valves, and the blood pressure within his right heart chambers was elevated (pulmonary artery systolic pressure of of 60 mmHg - normal is 25). So what were we to do?
The first step was to identify, or try to identify the cause of BH's cardiomyopathy. While viral infection may be the cause of cardiomyopathy in some individuals, there is increasing evidence that cardiac heavy metal overload is the culprit in many if not most cardiomyopathy patients. Lead and Cadmium have been implicated, but aren't likely the problem in BH's case, as these toxic metals are removed from the body with EDTA, and BH had received 264 EDTA treatments. However, EDTA does not remove Mercury, and MERCURY appears to be THE CARDIOMYOPATHY METAL. A recently published study looked at trace and toxic metal levels in heart muscle biopsy specimens in individuals with heart failure of various causes and in normal subjects. While the patients with decompensated coronary disease had five times as much myocardial (heart muscle) Mercury as did the normal subjects, the cardiomyopathy patients had 22,000 times more. This is not a healthful situation.
BH had had his Mercury amalgam fillings removed years ago, but he had not undergone a program of medical or nutritional Mercury detoxification. A packed red cell study demonstrated a markedly elevated intra-red cell Mercury level. We thus hypothesized that Mercury was playing a role in BH's deteriorating cardiac health. Then we came up with a treatment plan.
1st BH began to sleep on a 20 Gauss Magnetico negative field sleep pad, while taking DMSA (a Mercury binding agent), in a 11 nights on - 11 nights off treatment schedule. With this BH began to feel a little better. After two months of this pre-treatment, BH came to Toledo for MME. Magnetic field therapy and MME in particular have a number of physiologic effects that might help a damaged heart, and one is to enhance the clearance of Mercury and other toxic metals from the heart muscle. Dr. Bonlie demonstrated to me that sleeping on the negative field mattress pad enhanced the clearance of toxic metals via the kidneys, and synergized with the metal clearing effect of DMSA. With MME we are treating one organ system at a times, while with the sleep pad we are treating the entire body. It is logical that pre-treatment with the sleep pad and DMSA will enhance one's response to formal MME, and that has been Dr. Bonlie's experience.
2nd, while I had nothing to add to BH's nutritional program, I did feel he might benefit from some additional pharmacologic treatments. BH was concerned about side-effects and did not want any additional drugs. We argued about this a little and BH won (as he should - after all it's his body, not mine - we doctors have to keep this in mind).
3rd, after being shot down on the drug option, I offered BH MME - BH had done his homework on MME and was eager to proceed. BH completed 139 hours of MME over a two week period. Early on he noticed nothing, but then things began to improve. Between our office and BH's hotel was a Home Depot. BH devised a self-rating scale for himself based on the number of Home Depot aisles that he could walk before he ran out of breath. Early on BH didn't feel so hot just walking into the store. Towards the end of MME, he could stroll the aisles without difficulty (he also bought a lot of stuff he didn't need, then had to take it back to Maryland - Mrs. BH was none too pleased). Back home BH continued to increase his exercise level. He bought a new bike and is now riding up and down the hills that dot the Maryland countryside.
Subjectively, BH got better. We don't have a means of objectively documenting an improvement in BH's intracellular physiology (we would have to do heart muscle biopsies before and after MME - not practical or desirable). We did repeat BH's cardiac echo study, which (macroscopically) looks at heart performance. BH's echo looked a little better. Keeping in mind that echo interpretation is reader dependent and that the study may vary slightly from day to day, I felt that BH's ejection fraction had improved (15-25% pre and 25-30% post-MME). I felt that the degree of mitral valve insufficiency had decreased a little, and was convinced that the degree of tricuspid valve insufficiency had decreased a lot. The pulmonary artery pressure, reflecting right heart strain, fell from 60 to 40 mmHg.
There was thus subjective and objective evidence that BH had improved with 139 hours of MME. He will continue to sleep on the Magnetico sleep pad and will take DMSA intermittently. Travel to and from Toledo is a strain for BH (especially with all of the Home Depot stuff) but we may treat BH with more MME in the future.
9/05 Update - I called BH to see how he was doing. He wasn't in. He was out riding his bike, up and down hills, near his home in Virginia. BH's wife related that BH's functional status had improved further since completing MME one year earlier. This no longer surprises us. If we are stimulating the production and utilization of ATP energy within the heart cells, should we expect cellular repair to occur within a few weeks? If we really are stimulating cardiac stem cells to proliferate and migrate, shouldn't it take some time for the peak effect to occur? After all, how many months did it take for your heart to form up in the first place? In any event, BH is pleased with his persistent benefit from MME and so are we.
7/06 Update - BH's cardiovascular and functional status remains improved We'd like him to come up to Toledo for a booster of MME but he has too many other things going on.
MME for Recent Onset Dilated Cardiomyopathy - MV - 9/04
|
DATE |
EVENT |
| 10/03 | New finding of Left Bundle Branch Block (LBBB) on EKG, leading to: xxxxxEcho - EF 30% with global pump dysfunction nnnn vvvvvPersantine Stress Scan - falsely positive for coronary disease disease xx aaaaaAngiography - non-flow restrictive, £ 40% narrowings with an EF of 40-45% |
| 7/04 | Cardiac echo - EF 35-40% with findings of diastolic dysfunction and LVd 6.0 EKG - LBBB |
| 65 hours | 65 hours of MME through 9/22/04: Symptoms - Oxygen requirement decreased EKG - LBBB persists x xx Echo - EF normal with septal dsynchrony due to LBBB; LVd 5.4 |
| 85 hours | EKG - LBBB resolved Echo - Wall motion and EF unequivocally normal; LVd 4.5 |
MV's cardiac condition improved with MME. Thus MV was a technical success, but it was a sad success, as this delightful gentleman later passed on due to another disease state that we could not address. This 79 year-old non-diabetic, remote former smoker demonstrated the new finding of Left Bundle Branch Block (LBBB) on a routine EKG in 10/03. Electrical activation of the heart muscle occurs through two nerve bundles. Dysfunction of the right bundle may occur as a normal variant finding, but LBBB nearly always reflects cardiovascular disease (heart attack, cardiomyopathy, or long-standing hypertension are the usual culprits). MV had only minimal hypertension, and it was well controlled medically. A chemical stress test (Persantine Cardiolite) returned abnormal, worrisome for coronary disease. Angiography demonstrated only mild coronary narrowings and a moderate, generalized weakness of the heart muscle - the problem was not coronary insufficiency, but cardiomyopathy.
For purposes of our research, and to follow MV's response to MME, a cardiac echo study was obtained pre-MME and repeated at two points in his treatment course. The baseline study demonstrated enlargement of MV's left ventricle (major pumping chamber), to 6.0 cm. (normal is £ 5.5 cm.), with an ejection fraction (percent volume of blood that the heart ejects with each beat - normal is 50-55%) in the 35-40% range. Medical therapy with an ARB (Angiotensin Receptor Blocker) was continued and MV began MME. MV remained frail and fatigued, I believe more due his non-cardiac than cardiac problems, but his requirement for supplemental oxygen decreased a little. An echo study carried out after 65 hours of MME showed definite improvement. Cardiac pumping function had normalized and MV's left ventricle had decreased in size to 5.4 cm. The only residual abnormality of note was the presence of dysnchronous wall motion, due to the persistent LBBB conduction disturbance. MME was continued and by 85 hours MV's EKG had normalized. The LBBB conduction delay seen on MV's pre-MME tracing had resolved. We repeated MV's echo and now saw completely synchronous wall motion, and the left ventricle was a little smaller, now at 4.5 cm. The EPSS is our most reproducible echo measure or cardiac pump performance, and it decreased from 1.1 pre-MME to 0.5 on the final study (a low number reflects better pump function).
Sometimes patients with cardiomyopathy demonstrate spontaneous improvement. I've also seen LBBB EKG conduction disturbances come and go, but not often, and never as a result of medical treatment. We never felt that we could restore the function of damaged cardiac nerves. Well. Dr. Bonlie has shown me that many patients with diabetic neuropathy experience a reduction or resolution of symptoms and improved nerve conduction findings following treatment with MME, so in theory, why shouldn't MME improve function of the cardiac nerves? Following MME, Patient JR was able to stop the anti-arrhythmia drug that was slowing his heart rate down too much, without recurrence of the arrhythmia, atrial fibrillation, so maybe we are effecting cardiac nerve function. We will continue to research this possibility.
7/06 Update - Unfortunately MV passed away due to a non-cardiac illness.
Cadmium, Cardiomyopathy, Cancer, and Hypertension - What's a Cardiologist to do?
|
DATE |
EVENT |
| Abnormal stress echo studies in '97, '99, and '02 - resting pump function preserved | |
| 4/03 | Resting pump function abnormal - ejection fraction 40-45% |
| 5/04 | EF 25-35%, EPSS 1.4, restrictive filling pattern, and moderate mitral regurgitation |
| 5/04 | New onset atrial fibrillation ® angiography shows normal coronary arteries and a cardiomyopathy picture, with an EF of 25-30% and PCW of 17 mmHg. |
| 6/04 | Triple challenge abnormal for Cadmium, Lead, and Mercury |
| 12/04 | EF increased to 35-40% after 10 IV EDTA treatments and ongoing drug therapy |
| 0 hrs | EF 35-40%, EPSS 1.3, restrictive filling pattern, and MR 4 cm2 |
| 200 hrs | EF 40-50%, EPSS 1.1, reduced compliance filling pattern, and MR 2.2 cm2 |
| 1/05 | Feeling well ® Chemotherapy, Surgery, and Radiation Therapy |
| 6/05 | EF Normal, EPSS 0.8 - BP now too low and meds being decreased |
Mercury is the key cardiomyopathy toxin, but Lead also plays a role, and Cadmium is clearly not a girl's best friend, and this girl had all three. When I first met HS in 1997, her problems were high blood pressure, recurrent headache, and hypothyroidism; a recent breast biopsy had returned benign. Her resting cardiac echo study looked good - the valves were intact and the ejection fraction was normal - but with exercise, pump dysfunction developed. I felt that one or more of HS's coronary arteries was blocked. I offered her a diagnostic coronary angiogram, but HS was feeling well and she wanted to hold off. Repeat stress echo studies in '99 and '02 were likewise abnormal, but no worse than in '97, and HS was still feeling well. HS was not feeling well in 4/03; she was experiencing shortness of breath with moderate effort and her echo now demonstrated abnormal pump function at rest. Her BP were also climbing, and I was having trouble controlling it with drugs and nutritionals.
In 5/04 HS presented with increased shortness of breath. Her BP was 180/120. Frequent PVCs (premature ventricular contractions) were seen on her EKG, with regions of atrial fibrillation (rapid, irregular rhythm). Her ejection fraction by echo was down to 25-35%. HS had always tolerated cardiac meds poorly, but I twisted her arm to take Accupril (blood vessel dilator), Furosemide (potent diuretic), and Digoxin (reduces heart rate), and I pushed and shoved HS into a heart catheterization.
HS's coronary arteries were normal, but pump function was abnormal, consistent with the echo picture, with an angiographic ejection fraction in the 25-30% range. The blood pressure within her heart, the pulmonary capillary wedge pressure (PCW) , was elevated at 19 mmHg (normal is 5-8); this explained HS's shortness of breath. In retrospect, HS's cardiomyopathy had been brewing since '97. The impairment in pump function with exercise, that I thought was due to a blocked coronary artery, was really an initial manifestation of HS's cardiomyopathy. OK, so I got it wrong in '97 - what can I do to make it right in '04?
HS continued her nutritional and pharmacologic program, and I added Coreg, an anti-adrenaline b-Blocker that is of value in CHF due to coronary disease or cardiomyopathy. Given that heavy metal overload may play a role in cardiomyopathy and hypertension, a diagnostic triple challenge (measure urine metals following the administration of the metal binding agents EDTA, DMPS, and DMSA) was carried out, revealing large spills of Lead, Cadmium, and Mercury. HS's insurer had a policy to cover IV EDTA chelation therapy to address heavy metal overload (but they later stiffed me), so we began her on this agent, aiming at Cadmium and Lead. HS ordered a negative field magnetic sleep pad, and began a program of DMSA (gets Mercury) 500 mg at bedtime, 11 nights on, then 11 nights off. The idea here was to slowly and safely remove from HS's heart the toxic metals that I felt were likely playing a role in her hypertension and cardiomyopathy.
All was proceeding nicely, until HS was diagnosed with cancer of her left breast. The tumor had spread into the left arm pit region, but there was no evidence of metastasis to the brain, lung, or liver. Her surgeon and oncologist recommended initial chemotherapy to shrink the tumor, followed by surgery, and later radiation therapy to mop up any remaining cancer cells. The problem HS faced was that the chemotherapy and left chest radiation therapy that she needed to kill the cancer cells would likely also damage her already dysfunctional heart. HS was improving with IV EDTA and oral DMSA (her ejection fraction had increased to 35-40%), but we didn't have the luxury of time to slowly finish this process - her oncologist wanted HS to start chemo in two weeks.
What could I do to make a meaningful difference in two weeks, to turn a poor candidate for cancer treatment into an acceptable candidate? You guessed it - we switched from IV EDTA to MME. HS completed 200 hours, sleeping through most of it, and the next day began chemo (modified by her oncologist to be less cardiotoxic). Her echo picture changed within this brief time period. Systolic function (cardiac pumping function), measured by the ejection fraction and the EPSS value (you want to see an increase in ejection fraction and a decrease in EPSS) improved. Diastolic function, the ability of the heart to fill without producing shortness of breath, also improved (a "restrictive" pattern was replaced by an "impaired compliance" pattern). The degree of mitral regurgitation, a backflow of blood when the leaflets of the mitral valve are trying ton close, lessened, atrial fibrillation did not return, and PVCs became less of an issue. Systolic function, diastolic function, valve function, and electrical function all improved - all in a matter of weeks.
HS's medical and nutritional regimen will be continued and I will monitor her heart as she proceeds with cancer therapy. Her echo will be repeated in eight weeks. My hope is that her cardiomyopathy will continue to heal, but we will watch for problems related to chemo and radiation therapy. While Mercury, Lead, and Cadmium have all been associated with cardiomyopathy, it is Cadmium that has been most closely linked to reproductive organ malignancy. First, Cadmium is toxic to your DNA, it is mutagenic. Second, Cadmium damages the enzyme that is tasked to repair damaged DNA (your "biochemical spell checker). Mother Nature knows that toxic substances might damage our DNA, so she gave us the spell checker as a safe guard, but she never anticipated that we would be exposed to Cadmium. Third, breast cancer (and prostate cancer) are estrogen driven, and CADMIUM STIMULATES THE ESTROGEN RECEPTOR. In animal studies, if you supply Cadmium to an animal who has had her ovaries removed, breast and uterine tissue will grow. If you supply Cadmium to a pregnant animal, her offspring will exhibit premature puberty. The incidence of reproductive organ cancer is skyrocketing; it is my opinion that Cadmium is playing a key role.
HS will continue to take DMSA, which removes Cadmium, Lead, and Mercury, and she will continue with the magnetic sleep pad. HS's surgeon and oncologist are going to cut our or kill the cancer cells in her body, and I'm going to remove the toxins that damaged her immune system and DNA in the first place. We all want HS to get better and then to stay better - the way to do this is to combine the best of standard medicine with the best of nutritional/complimentary medicine, and this is the medicine that HS is receiving.
6/05 Update - To this point HS has received 5 or a planned 6 cycles of chemotherapy, which she has tolerated reasonably well. Her echo was repeated, now 6 months out from MME, and demonstrates further improvement. The EPSS is now normal, at 0.8, and her ejection fraction is now normal. By echo, her heart now looks like that of an individual with treated hypertension. Speaking of hypertension, HS's BP has been falling, and is now too low. HS's diuretic was discontinued and I am now cutting back on her other cardioactive drugs. Her response to chemotherapy has been positive. Not only has her heart not been damaged by the chemotherapy, during this time interval it has improved further.
7/06 Update - HS completed chemotherapy, and then underwent surgery, without difficulty. Prophylactic radiation therapy was carried out in late '05. A paper came out, with much media fanfare, regarding the benefits of a new chemotherapeutic agent, Herceptin, in reducing the recurrence rate of breast cancer. We all wanted HS to remain cancer free, so HS received Herceptin in 12/05. While standard chemotherapy had not compromised HS's heart, Herceptin did. She went back into atrial fibrillation, mitral regurgitation developed, and her ejection fraction dropped down into the 30-35% range. Herceptin was stopped, medical therapy was advanced, Bioresonance Therapy initiated, and HS received an additional 100 hours of MME to her heart. Her ejection fraction rose into the 40-50% range by 3/06, and she converted back to normal sinus rhythm in 6/06. Her echo will be repeated later this summer and it will problem look great.
12/06 Update - HS's EF is now back to normal.
Racing against the (Defibrillator) clock - RD - 4/05
|
ATE |
EVENT |
| '01 | Unexplained fatigue - EF 55% by cardiac echo |
| '02 | Normal 10:07 stress echo study |
| 6/04 | Ejection fraction reduced at 41% by nuclear study Chemical stress perfusion study negative for coronary artery disease |
| 9/04 | EF down to 35% by echo with PVCs and + T wave alternans test Þ Implantable defibrillator and possible biventricular pacemaker recommended |
| 4/05 | EF 40-45% by echo after 24 hours of MME |
| 5/05 | EF 45-50% after 242 hours MME - Feels great |
RD was not critically ill when I first saw him in April '05, but he was under a time constraint. RD was in a hurry to get better. Permanent defibrillator implantation, possibly with concomitant biventricular pacemaker placement, had been recommended. RD wanted time to think things over and/or to improve to the point where this hardware would not be necessary. RD's cardiologist and electrophysiologist agreed to give RD some time, but they were concerned about his status, and asked him to come to a decision. RD was thus in a hurry to get better.
RD is a health conscious 78 year old. Exercise has been a regular part of his life. RD doesn't smoke and he's always followed a prudent diet. RD's Cholesterol is only 207, and his homocysteine, Lp(a), ferritin, fibrinogen, and CRP levels are all low. RG has undergone over 100 IV EDTA treatments, so Lead or Cadmium overload is not likely. All but one amalgam filling have been removed, but RD has not undergone medical Mercury detoxification, of interest here given the link we have previously discussed between Mercury and dilated cardiomyopathy.
RD was feeling poorly in '01; nothing specific, just a sense of fatigue. A cardiac echo was carried out for screening purposes, and returned normal, with an ejection fraction of 55%. The next year RD breezed through a 10:07 stress echo study (an exceptional treadmill time for a then 75 year old). In 6/04, things weren't looking so well. A nuclear scan demonstrated pump dysfunction; RD's ejection fraction was down to 41%. A stress study, this time with a chemical stress agent, returned negative for coronary disease. The diagnosis of dilated cardiomyopathy was made. Three months later RD's ejection fraction had fallen further, to 35%, and extra beats, PVCs, were seen on his EKG. The presence of a rhythm disturbance in a cardiomyopathy patient with pump dysfunction worries us. We worry about the potential for a sustained or life-threatening rhythm disturbance - we worry about the potential for sudden death. RD's doctors wanted RD to undergo a heart catheterization along with an invasive electrophysiology study (best test to see if a potentially life-threatening rhythm disorder is actually present), but RD wanted to remain non-invasive. A T-wave alternans test, the best non-invasive test for arrhythmia susceptibility, was carried out and returned abnormal. RD's doctors recommended implantation of an implantable defibrillator, possibly with concomitant placement of a biventricular pacemaker (synchronizes contraction of the left and right heart and on this basis increases ejection fraction and overall cardiac performance).
RD wasn't enthusiastic about all this hardware being placed in his body. RD began an extensive cardiac nutritional program, including agents such as L-Carnitine and Co-Enzyme Q, both of which have been shown to improve pump function and decrease mortality in patients with cardiomyopathy. He also wasn't ignoring the advice of his doctors. He took his prescription drugs, as much as his blood pressure would tolerate, and his plan was to undergo defibrillator implantation if his heart function did not improve.
RD heard about MME from a physician who I work closely with. RD looked through our website and we spoke over the phone. RD was in a hurry to get started. Our first opening was on a Saturday night and RD took it. Thus his baseline, pre-MME echo was actually obtained after two nights of MME treatment. It looked better than his most recent exam of 9/04. This improvement might be due to the 24 hours of MME that RD had received, but RD's nutritional program may also have played a role (probably did). Given RD's time constraint, we did not pre-treat him with two moths of combined DMSA and negative field sleep pad therapy, but RD received two 500 mg doses of DMSA, a Mercury chelator, with each MME treatment. RD tolerated MME well. His blood pressure fell a little, not unexpected as magnetic field therapy has been shown to increases the formation of Nitric Oxide, our bodies natural arterial dilator; and to decrease the production of Aldosterone, a salt and water retaining hormone. RD cut back on his meds and his BP stabilized. We didn't see any PVCs on the EKG we did, and after 242 hours I felt that RD's ejection fraction was nearly normal, in the 45-50% range. Post-MME RD will sleep on a Magnetico negative field only pad, and he'll keep up with a DMSA-based Mercury detoxification program (we think that MME drives Mercury out of the heart, but if we don't detoxify the rest of the body, Mercury and other toxins will leave the other internal organs and re-poison the heart). In several months resting and stress echo studies will be carried out, to make sure that we have gotten the job done. Our hope is that the combination of MME with nutritional and targeted drug intervention will make the defibrillator and pacemaker unnecessary. After all, who wants to be a tin man if instead you can be magnetized.
7/06 Update - RD is now 15 months out from MME and he continues to feel well. RD works out regularly on his treadmill, maintaining a speed of 3.5 MPH. When RD gets some free time he will come to Toledo for a follow-up cardiac echo and re-evaluation. A metal challenge study will be carried out to make sure that we have cleared all the Mercury out of RD's system, and I will discuss with RD what we are learning about Medical Bioresonance and Bone Marrow stem cell mobilization, techniques not available to us when RD underwent successful MME in 4/05.
MME for Chronic Dilated Cardiomyopathy - BR - 11/4
|
DATE |
EVENT |
| '99 | Sudden onset congestive symptoms xxxxxxxx EKG - LBBB xxxxxxxx Angio - normal coronary arteries - severe pump dysfunction |
| 9/04 | Stroke while anticoagulation on hold for transplant work-up |
| 9/04 | Heart cath - PCW 31 and PAs 85 mmHg, falling to 24 and 60 mmHg on Milrinone |
| 10/04 | Echo on Milrinone - EF 10-20%, EPSS 3.6, severe mitral regurg, & PAs 45 mmHg |
| MME | 200 hours planned - MME stopped at 61 hours due to PIC line sepsis, requiring hospitalization. 20 additional hours provided post-discharge for a total of 81 hours |
| 11/04 | EKG - LBBB without change Symptoms - unable to evaluate; still recovering from sepsis Echo off Milrinone - EF 15-20%, EPSS 3.0, severe MR, & PAs 55 mmHg |
BR had not had much luck with his heart, and that bad luck continued during his visit to Toledo for MME. This 56 year-old non-hypertensive, non-diabetic, amalgam bearing non-smoker experienced sudden onset shortness of breath in 1999. Catheterization demonstrated findings of cardiomyopathy (advanced pump dysfunction with normal coronary arteries). BR proved to be quite sensitive to the side-effects of our usual medications, but he put himself on an extensive nutritional program (Mrs. BR researched this area fully and knows her nutritional stuff), and over the years he did well.
BR's physicians were following the course of his cardiomyopathy with yearly cardiopulmonary stress studies. This year's study didn't look so good, and BR was advised to undergo evaluation for possible cardiac transplantation. BR's routine anticoagulant was put on hold to allow a lower GI study, and while off this agent BR sustained a stroke. BR's cardiac condition had never kept him from working, but the stroke did. Subsequent heart catheterization revealed a pulmonary capillary wedge (PCW) of 31 mmHg (Normal is 5-10; this reflects fluid buildup behind the left heart. The PCW is the pressure the lungs "see"; the higher your PCW, the more short of breath you will be with effort and at rest). His pulmonary artery systolic pressure (PAs) was 85 (Normal is 25; an elevated PAs reflects strain experienced by the right heart). Infusion of Milrinone (an adrenaline like agent that whips the heart and causes it to beat more forcefully - it is useful in acute heart failure but long-term it may overwork the heart, compromising long-term outcome) lowered the PCW to 24 and the PAs to 60, so the decision was made to place a PIC line (percutaneous intravenous catheter - an IV placed at the level of the elbow and advanced into the heart, allowing long-term IV therapy) and to send him home on chronic IV Milrinone.
The stroke put the kabosh on the concept of cardiac transplantation. Dual chamber pacemaker/Cardiac defibrillator implantation was offered to BR (and this is not a crazy idea - I've sent many patients for this procedure), but pacemaker implantation would close the door forever on MME. BR wanted to come to Toledo and undergo MME before undergoing more procedures; at that time he was clinically stable and this plan made sense to me.
While reading BR's pre-MME echo, the thought entered my mind that BR's echo "was the worse I had ever seen outside of a cardiac arrest". When we resuscitate you from cardiac arrest in the hospital, a bedside echo study is often done, looking for a mechanical problem or fluid collection around the heart that may have caused the arrest. At that point, the just-back-from-the-dead heart demonstrates incredibly poor pumping function. Well, that was what BR's echo looked like pre-MME, despite the IV Milrinone cardiac whip. Frankly I was amazed that BR was even walking and talking.
BR began MME without incident, and after 22 hours I decreased his Milrinone dose by 25%, and with this BR had no difficulty. My plan was to wean the Milrinone off slowly as BR proceeded through a planned 200 hour MME program. That was the plan, but three days later, at 61 hours of MME, BR experienced the sudden onset of shaking chills and nausea. This didn't sound like a cardiac problem; it sounded like an infectious problem. BR's indwelling PIC line had become infected. BR required hospitalization. Gram negative bacteria grew out of his blood, and the septicemia threw him into frank heart failure. Antibiotic therapy was initiated, his anticoagulant was put briefly on hold to allow removal of the infected PIC line, and (miraculously in my opinion - gram negative sepsis is tough on otherwise healthy individuals and BR was anything but healthy) BR recovered. Post-hospital discharge BR received 20 additional hours of MME, but then had to return home, due to some pressing family responsibilities. We repeated his echo, post-sepsis, and now off Milrinone, and it actually looked a little better. BR's ejection fraction had increased slightly, and the EPSS value, our most reproducible echo measure of pump function, had fallen from 3.6 to 3.0 (normal is 1.0 or less). Under the circumstances, I was pleased with this result. After BR recovers further from his stroke and PIC line sepsis, and after his family matters have been attended to, we are hopeful that BR will return to Toledo so we can finish the MME program that we started. Hopefully, without gram negative sepsis and the whipping action of Milrinone to contend with, he will respond more favorably to MME.
7/06 Update - BR did not return to Toledo for additional MME - he just didn't feel comfortable taking more time away from family and his work, and his health such that travel was no longer possible. A biventricular pacemaker was placed; later he developed atrial fibrillation that led to a prolonged hospitalization. Cardiac transplantation was carried out in 3/05 with excellent results; BR is now back to work. This is a good result, but the means to achieve it were certainly difficult for BR and his family. I wish that we had had the opportunity to treat him with a full 200 hours of MME as originally planned.
Fixed and Vasospastic Ischemic Cardiomyopathy with Persistent Symptoms - SA
|
DATE |
EVENT |
| '96 | Initial inferior wall heart attack ® Three vessel Bypass surgery |
| 1/99 | Abnormal 8:37 stress echo ® All 3 native arteries occluded but all grafts open; chest pain responsive to Arginine (endothelial dysfunction likely the culprit) |
| 12/00 | Non-ischemic 5:30 stress cardiolite study |
| 11/02 | Abnormal 8:00 stress echo |
| 12/02 | Rest pain ® All 3 grafts remain open but high-grade narrowings now present in the two terminal branches of the RCA, beyond the touchdown site of its vein graft |
| 12/02-1/03 | 35 hours EECP - Angina resolved with a non-ischemic 6:06 (effort limited by hip pain) stress echo study |
| 8/03 | Anterior wall heart attack - No new narrowings - Normal blood supply to the damaged region - Vasospasm and/or clot formation the culprit |
| 7/04 | Class III angina and compensated CHF, on meds, with EF 25-35% & EPSS 1.9. |
| Fall '04 | Magnetico sleep pad + DMSA for 2 months, then 150 hours MME: Angina Angina improved bbbb Echo Echo - EF 30-40% & EPSS 1.0; diastolic function improved im |
| 9/05 | Clinically stable with
quiescent angina Echo - EF 35-45% & EPSS 1.0; left atrial size decreased |
SA had sustained two heart attacks, the 1st on the basis of an obstructed artery; the 2nd due to vasospastic/thrombotic occlusion of an anatomically normal bypass graft. SA remained troubled by effort angina, pump function was impaired, and triple-drug heart failure therapy was just barely getting the job done - so we treated him with MME and he got better.
In 1996, SA experienced a heart attack involving the back wall of his heart, due to obstruction of the Right Coronary Artery (RCA). His Left Anterior Descending (LAD) and Circumflex (Circ), serving the front and side walls of the heart respectively, also contained narrowings, so triple graft bypass surgery was carried out. SA's recovery was uneventful.
Symptoms recurred in early '99. A stress echo study carried out by SA's
prior cardiologist returned abnormal, showing scarring over the inferior wall
(expected) and impaired post-exercise wall motion over the front wall (not
expected). Angiography revealed that all three native vessels were
occluded, but that their bypass grafts were widely patent. The finding
of normal grafts suggested that the stress echo study was misleading and that
SA's pain was not cardiac in nature, but it persisted. SA sought my
counsel and I put him on Arginine, and his pain resolved. Arginine is
the raw material that the artery lining endothelial cells take up and convert
into Nitric Oxide, our natural blood vessel dilator and blood clot preventer.
SA's good response to Arginine suggested to me that SA's angina was present on
the basis of endothelial dysfunction (similar to our 1st case study -CR).
Chronic hip pain on the basis of arthritis worsened in the fall of '02. A stress echo study carried out by myself returned abnormal, and turned out to be accurate, as two months later SA was experiencing pain again. Angiography again demonstrated all three native arteries to be occluded and all three bypass grafts to be patent. Unfortunately, "distal disease" had developed since '99. Flow restrictive narrowings were now present in the two terminal branches of the RCA (so even though its vein graft was open, the still viable heart muscle in the RCA distribution was not receiving an adequate blood supply). These narrowings were too deep within the artery to be reached by the angioplasty catheter, so we treated SA with EECP. His chest pain resolved, just as we expected, in a patient with patent grafts and two intact distal arteries to generate collaterals from. A stress echo study was carried out post-EECP, to check our work before SA underwent hip replacement, and it looked good.
SA underwent uneventful hip surgery in the summer of '03. That fall, SA presented with chest pain accompanied by EKG and lab findings consistent with a heart attack involving the front wall of SA's heart (recall that the grafts to the front and side walls of SA's heart were wide open in 12/02, so this wasn't expected). SA received IV nitroglycerin and heparin (an IV blood thinner) in the emergency room, and was then transported directly to the cath lab. We were expecting to see a new narrowing in the the vein graft supplying the front wall of SA's heart, but instead say a normal vein graft; SA's vessels hadn't changed a bit since 12/02. The distal narrowings in the RCA had been collateralized by EECP and were a non-issue - from the perspective of the heart attack that damaged the front wall of SA's heart, his invasive study was "normal". Well, even though the study was "normal", SA had sustained considerable damage. His ejection fraction (percentage of blood that the heart ejects with each beat - normal is > 50%) was down to 30%'s. Heart failure was now an issue; it improved but did not fully resolve with increased drug therapy. Just how and why SA sustained this "normal artery" heart attack is something that I cannot fully explain. Presumably the vein graft went into spasm, a state of focal, severe, endothelial dysfunction, or a clot formed within the graft - we'll never know because the graft was open (but the damage already done) when we cathed him. To be sure, I left SA on a regimen designed to maintain endothelial integrity, and added Nattokinase, an blood clot dissolving agent that is active orally.
SA hasn't had any more heart attacks, but he continued to experience angina with mild effort, and his stamina remained low. SA has Mercury amalgam fillings and a diagnostic DMPS challenge study had demonstrated Mercury overload, which we had previously not addressed (see discussion in Preparation & Nutritional Support section). SA began to sleep on a Magnetico negative field pad in the early fall of '04, taking DMSA in an 11-night on, 11-night off regimen. SA then underwent 150 hours of MME, taking DMSA with each session. His other treatments were continued.
SA's chest discomfort resolved fully with MME. I spoke with him 4 weeks later and he indicated that he was having some discomfort but overall felt better (see his description), and I will be seeing him shortly, and will try to determine whether his current symptoms are heart or non-heart in causation. Echo studies were carried out before and after MME. I felt that SA's pumping function had improved, with a decrease in EPSS (our most reproducible echo measure of pump function) from 1.9 to 1.0, and a rise in ejection fraction from 25-35% into the 30-40% range. Diastolic function, the ability of SA's heart to fill normally, also looked a little better.
SA will continue to sleep on the negative field pad, and will take DMSA 7 night a month. I will see him to evaluate his current symptoms, and we may carry out a stress study, to help differentiate heart from non-heart discomfort.
SA described his MME experience as follows:
"Initially after treatment the angina I had been encountering was gone for 4 or 5 days. It has returned with no improvement noted. However, my overall feeling and "energy level" is better. I've had less swelling in the lower part of my legs. I've an idea that my IBS (Irritable Bowel Syndrome) has improved somewhat. Hard to tell for sure. Arthritis which gives me problems depending on weather conditions hasn't changed much." Note - we treated only SA's heart, not his joints or GI tract.
7/06 Update - SA remains improved, and has not required a hospital stay or invasive study since completing MME in 10/04. Echo study carried out in 9/05, one year out from MME, looks a little better, with a slight improvement in pump function and a decrease in left atrial chamber size.
Cardiomyopathy, Atrial Fibrillation, and Mitral Regurgitation - TM - 4/05
|
ATE |
EVENT |
| 1/05 | CHF - Atrial Fib, EF 40%, and moderately severe mitral regurgitation |
| 2/05 | Normal coronaries, EF 40%, PCW 15 mmHg, but only mild MR |
| 2/05 | Echo - Normal EF, moderate MR |
| 4/05 | Amiodarone initiated + 207 hours of MME |
| 6/05 | Feels better, MR still moderate by echo, and still in Atrial Fib |
| 7/05 | Back to Normal Sinus Rhythm |
TM presented in 1/05 with 6 months of progressive shortness of breath and fatigue. On exam, crackles could be heard over her lung fields, consistent with fluid accumulation behind the left heart, and her neck veins were distended and ankle edema was present, consistent with fluid accumulation behind her right heart. TM was in congestive heart failure (CHF). What was the cause? TM had been troubled by hypertension, but with medical therapy her blood pressure had been well controlled. Her pulse was irregular, and an EKG demonstrated her rhythm to be Atrial Fibrillation (irregular, uncoordinated rhythm that compromises pump function by 20-40%). A cardiac echo study demonstrated impaired pump function, with an ejection fraction (EF) of 40%, and what looked to me to be moderately severe mitral regurgitation (leakage of the valve between the left ventricle pump and its atrial storage chamber, promoting fluid buildup within the lungs and shortness of breath). Her clotting chemistries were abnormal, consistent with liver dysfunction due to CHF (blood backs up behind the right heart, distending the liver, compromising its ability to manufacture clotting factors). Drug therapy for CHF cleared the retained fluid, but compromised TM's kidney function; her creatinine rose. Adjustments were made, and we arrived at a regimen that compensated TM's CHF without adversely affecting her kidneys.
At this point I couldn't tell which of the three abnormalities present (Atrial Fib, Mitral Regurgitation, or Cardiomyopathy) was the primary problem and which were its consequences - so I treated all three. Heart catheterization revealed normal coronary arteries, pump dysfunction with an EF of 40%, and what appeared to be only mild mitral regurgitation. The blood pressure within TM's heart, the pressure that her lungs are exposed to, the PCW (pulmonary capillary wedge pressure), was elevated at 15 mmHg (normal is 5-8), consistent with her complaint of shortness of breath with exertion. With respect to grading the severity of the mitral regurgitation, there was disagreement between the echo and catheterization assessments. TM's echo was repeated following the catheterization, and revealed now normal pump function, and what I felt to be moderate mitral regurgitation (our methods of assessment don't always agree 100%, and as all of this was going on, TM's CHF was responding to treatment). She remained in Atrial Fibrillation, and at this point my feeling was that this rhythm disturbance had been her primary problem all along. Thus I offered her several approaches to deal with it. TM had earlier been placed on coumadin anticoagulation to prevent clot formation within her fibrillating atria. What steps could be taken next?
1. Simply leave her in Atrial Fibrillation and focus on heart rate control - but this would leave her with impaired cardiac performance and a life-long requirement for coumadin anticoagulation.
2. Carry out electrical cardioversion - this might work but if her underlying condition was not changed, why wouldn't the rhythm disturbance return?
3. Begin drug therapy with Amiodarone. This is our most effective anti-arrhythmic agent, but it takes two months to work and has side-effects. If it doesn't work by itself, having the drug on board increases the likelihood that electrical cardioversion will be successful.
4. Refer her to the Cleveland Clinic for Atrial Fib ablation (using a catheter to destroy - with pinpoint precision - the nerve pathways in the atrial that sustain the fibrillation). Several of my patients have done well with this technique and are now off anti-arrhythmic drugs and Coumadin anticoagulation.
5. Begin MME, aiming to improve heart function and drive out any heavy metals that may be playing a role in her cardiac dysfunction (TM did have Mercury amalgam fillings).
TM chose to begin Amiodarone at a low dose (a good idea with her sensitivity to cardiac drugs) and to undergo MME. TM completed 207 hours of treatment. Her immediate post-MME echo picture was unchanged, and she remains in Atrial Fib, but she felt better (see below). We are learning that the peak benefits of MME may not be obvious for several months, and we also know that it takes Amiodarone several months to work. Our plan will be to continue drug therapy, and arrange for an electrical cardioversion procedure. If that doesn't work, then arrangements will be made for Fib ablation in Cleveland. The wait time for this procedure is 6 months, and TM just might convert to normal rhythm on her own during this time interval.
TM's evaluation - "Prior to starting MME treatment I was feeling tired and slightly irritable. My energy level was low. Since completing the MME sessions I feel more calm and have noticed an improvement in energy as I am anticipating undertaking tasks previously avoided. There has also been a noticeable change in my temperament and interactions with family members".
2 months Update: TM's rhythm is now back to normal. It appears that we need to be patient, and give time for MME to have an affect on a cardiac rhythm disturbance, just as we do with a cardiac pump dysfunction or a and neurological impairment. TM's quote - "Thank You for MME".
7/06 Update - TM continues to do well on all cardiovascular fronts; atrial fib has not recurred.
MME for Progressive Cardiomyopathy - SM - 10/05
|
DATE |
EVENT |
| 2/04 | Echo - EF 30%; LVd 6.2, LVs
.4.4, and LA 3.9 cm. Holter - 6,700 PACs over 24 hours |
| 3/04 | Normal coronary arteries - angiographic EF 30% |
| 9/04 | Echo - EF 25-35%; LVd 6.8, LVs
5.0, and LA 4.2 Holter - 15,637 PACs, runs of SVT, and 1,043 PVCs |
| 4/05 | Echo - EF 20-30%; LVd 7.9, LVs 5.9, and LA 4.0 |
| 8/05 | 20 Gauss sleep pad with 30 days TD · DMPS - Glutathione |
| 10/05 | 200 hours MME with oral DMSA |
| 11/05 | Echo - EF 30-35%; LVd 6.7, LVs 5.0 and LA 3.4 cm. |
| 5/06 | Echo - EF 30-40%; LVd 6.2, LVs 4.3 and LA 3.8 cm. |
SM presented in 2004 with classic signs and symptoms of dilated cardiomyopathy: palpitations, shortness of breath with effort, an enlarged left ventricle with poor pump function, normal coronary arteries, and cardiac arrhythmia - over 15,000 premature atrial and 1,000 premature ventricular beats over a 24 hours period. Drug therapy (ß-Blocker, ACE Inhibitor, ARB) was tried, and was poorly tolerate - she felt worse, not better - all SM could tolerate was low dose Coreg at 12.5 mg twice a day. Carnitine, Co-Enzyme Q, antioxidants, fish oil, and mineral supplementation was well tolerated and was included in SM's program.
SM worsened over the following 14 months. Her energy level fell, pump function deteriorated, and her left ventricle enlarged further (left ventricular diastolic dimension increased from 6.2 to 6.8 to 7.9 cm., while the systolic dimension increased from 4.4 to 5.0, to 5.9). The left atrium also increased in size. I tried different drugs but SM just couldn't take them. My standard drug and nutritional approach to dilated cardiomyopathy was not working, so we switched to a program of detoxification and MME. Previously SM had received over 100 IV EDTA treatments; Mercury amalgam fillings had been removed but she had not undergone Mercury chelation with DMSA or DMPS.
SM slept on a 20 Gauss Magnetico negative field only sleep pad for two months. She applied transdermal DMPS-Glutathione to her skin every other evening over the first month (two months of DMPS were planned but we got our signals crossed). SM then received 200 hours of MME over 17 evenings, receiving DMSA, 500 mg, twice each session.
SM was just finishing MME as of the time of this writing; she is tired from spending the last 17 nights with us so it is difficult to say whether she feels better or not. Her echo looks better; the chambers are smaller and pump function has picked up (see graphic). We expect to see further improvement, in terms of SM's echo picture, and symptoms, over time - and we did:.
7/06 Update - SM's left heart chamber dimensions did decrease with MME; the LV diastolic dimension from 7.9 to 6.7 cm, and the systolic dimension from 5.9 to 5.0 cm. But stem cells, activated by MME, take time "to grow up" (at least this is our theory). Echo studies carried out 2 and 7 months out from MME show further improvement - this is no longer a surprise to us - rather it is the expected finding. Clinically SM continues to do well; her symptoms are stable and she has not required a hospital admission.
55 Pounds of Edema Fluid lost in 25 days - HR - 5/05
|
DATE |
EVENT |
| '94 | Heart Attack - RCA 100%, other arteries diseased - bypass surgery declined |
| 3/02 | CHF - EF 15-25% with moderate mitral regurgitation |
| '02 | EECP carried out - felt better and EF rose |
| 5/22/06 |
Echo - EF 20-25%; EPSS 2.5, severe MR, severe TR, moderate pericardial
effusion Wgt. - 215 lbs. Clinical - Gross CHF with edema to waist, short of breath at rest, required oxygen |
| 5/22/06 |
Medical therapy adjusted 300 hour program of MME initiated Bioresonance therapy initiated |
| 6/9/06 |
Echo - EF 25-35%; EPSS 1.8, mild MR, mild TR, moderate pericardial
effusion Wgt. - 162 lbs. Clinical - Edema minimal, short walks without difficulty, oxygen now intermittent |
| 6/9/06 | Stem Enhance added |
| 6/16/06 |
Echo - EF 30-35%; mild MR, mild-moderate pericardial effusion Wgt. - 159 lbs. Clinical - Walks 5 loops around the office without major difficulty |
HR is a delightful, intellectually and physically independent, and nutritionally aware 75 year old who lives in Vermont. HR sustained a heart attack in 1994. One artery was occluded; another contained a high grade narrowing and the third a moderate blockage. Bypass surgery was advised but BR had other ideas (Doctors do not win arguments with HR). HR put himself on a well thought out and complete nutritional program and did great for many years. HR's condition worsened in 2002; he probably had a second heart attack. HR was hospitalized with congestive heart failure (CHF). Shortness of breath and edema cleared with diuretic therapy. Cardiac echo described an ejection fraction of 15-20% with moderate mitral regurgitation. Following his recovery HR underwent EECP in Vermont; his exercise capacity improved and his ejection fraction rose to 40%. HR did well for several years.
HR's congestive symptoms became more of an issue in early '06. All of a sudden he had to sleep with his head up at night. Walking and fishing (HR's passion) were now difficult to carry out. HR's son, a medically and nutritionally aware respiratory therapist, saw what was going on and advanced his Dad's nutritional program. HR learned about MME in a health newsletter, studied this website, and gave me a call in early May '06. HR and his son then spent three weeks in Toledo as HR received 300 hours of MME.
When I first met HR on 6/9 my first thought was "I'm going to have to admit this man to the hospital". HR was short of breath at rest, his legs were huge with edema fluid up to the level of the thigh, and he couldn't walk across the room comfortably. Cardiac echo showed a dilated, dysfunctional heart with moderate to severe regurgitation across both the mitral and tricuspid valves, and a fluid collection (pericardial effusion) surrounding the heart. HR is not enthusiastic about drug therapy, but he allowed me to advance his diuretic, add in Spironolactone and Coreg (both block hormones that whip the heart in CHF patients). HR was already on an extensive nutritional program, including Co-Enzyme Q and Carnitine; Ribose was added to enhance ATP energy production. MME was initiated and HR improved, and he improved rapidly.
A lot of edema fluid was mobilized. As of 6/02, HR had received 125 hours of MME; his weight had fallen from 215 to 177 pounds. HR was now able to walk short distances with less distress. HR's echo was repeated on 6/9. At this point HR's weight was down to 162. HR's ejection fraction had increased from 20-25% in to the 25-35% range, and of greater importance, the severity of mitral and tricuspid regurgitation had decreased. HR's heart was now less enlarged, the valve apparatus could now function more effectively, so the valve dysfunction had lessened. These pump function and mechanical improvements translated into a marked improvement in HR's functional status. He felt better, he looked better, and he could do more.
At this point our first order of Stem Enhance arrived. Stem Enhance is a nutritional agent that mobilizes uncommitted, pluripotential stem cells from the bone marrow in to the circulation (blood levels rise by 27%). These cells, sometimes described as CD34+ cells, can "land" within a dysfunctional organ and hopefully participate in its functional recovery. Stem Enhance is not a drug, it is not an FDA approved agent, but the use of Stem Enhance in the people who we treat with MME makes sense (I take it and love the stuff. I am 50 but am now running as if I was 30 again - 16 miles up to three days a week with much less muscle soreness and fatigue). Stem Enhance was added, HR continued his nutritional and pharmacologic program, and he completed another 175 hours of MME.
HR's weight was down to 159 lbs. at this point, down 55 lbs. since beginning his MME program. We have a large office, stuffed full of EECP, MME, cardiac echo, and other machines and offices. Before beginning MME, HR could barely walk in from the car; now HR can briskly walk the outer loop of the office five times. His ejection fraction was in the 30-35% range, and valvular leakage remained only mild. Our plan will be for HR to complete a four month program of Bioresonance Therapy, and to remain on Stem Enhance for an additional three months. In six months HR's echo could be repeated, and hopefully we will see an additional improvement. In the meantime, HR will busy himself fishing.
A Big Man with a No Longer Big Heart - EN - 6/06
|
DATE |
EVENT |
| 1/03 | Atrial Fibrillation ® Electrical cardioversion and Sotalol ® Normal rhythm |
| '04 | Kidney and liver toxicity ® Amiodarone substituted for Sotalol |
| 1/05 | CHF - EF 30%, 50% branch vessel narrowing; RA 15 mmHg and PCW 27 mmHg |
| 8/05 | Echo - EF 45-50% with severe left ventricular hypertrophy |
| 9/05 |
Echo - Dilated (LVd 6.3, LVs 4.7 cm), hypertrophied, stiff left
ventricle; EF 45% DMSA therapy initiated |
| 12/05 | Bioresonance Therapy initiated |
| 6/11/06 | MME and Stem Enhance begun |
|
6/21/06 150 hr |
Echo - LVd 6.4, LVs 4.0, hypertrophied, stiff left ventricle; EF now normal |
|
6/29/06 300 hr |
Echo - LVd 4.9, LVs 2.8; LV still hypertrophied and stiff but EF now
increased Clinical - Feels well, weight down from 319 to 302 |
| ® | Continue Stem Enhance, DMSA, and repeat echo in 3 months |
EN is a big man - he looks like a retired professional athlete. EN is also a nice man; he goes out of his way to make the people around him feel comfortable. He shows his appreciation when others help him. You might describe EN as "big hearted", and you would be right, in more ways than one. EN had an enlarged, abnormally thickened, and dysfunctional heart. But now you would be wrong, as EN has undergone 300 hours of MME and his heart is now normal in size - but he's still "big hearted" in attitude and spirit.
EN is health conscious and health aware. Recognizing the role of toxicity in the age-related degenerative disease states that plague our society (and which will bankrupt our health care delivery system), EN had previously undergone 100 IV EDTA chelation treatments. EN had his amalgam fillings removed (a few were left behind, underneath crowns, and became exposed when the crowns fell off). EN has followed a comprehensive nutritional program, and he has worked with nutritionally oriented physicians.
Thus EN and his doctors were surprised when he developed atrial fibrillation in 1/03. EN was anticoagulated, begun on Sotalol (an anti-arrhythmic agent) and then electrically cardioverted back into normal rhythm. Liver and kidney problems developed and were felt to be Sotalol related; this agent was dropped in favor of Amiodarone, another anti-arrhythmic. EN did well until 1/05, when he presented with biventricular heart failure. Edema fluid and shortness of breath cleared with diuretic therapy. Cardiac catheterization demonstrated only modest coronary disease. The problem was Cardiomyopathy - EN's heart was enlarged, stiff, the wall was thickened (hypertrophied), and pump function was off, with an ejection fraction of only 30% (50% is normal).
I began working with EN in the fall of '05. His ejection fraction had improved into the 40-45% range, but his heart was still enlarged, thickened, and stiff. Bioresonance Therapy was initiated, along with oral DMSA (binds Mercury, which would not have been removed by the EDTA that EN had received previously). EN remained on the go, traveling a lot, and working every day that he was not traveling (EN's supposed to be retired but he loves his work).
EN was able to carve out time to come to Toledo for MME in 6/06. He received 300 hours of MME over 20 days. EN received two doses of DMSA with each 10-12 hour MME session, and he was begun on oral Stem Enhance.
An echo taken at 150 hours compared favorably to EN's fall '05 baseline.
Pump function was now normal, the left ventricular systolic dimension (the
heart fills in "diastole" and contracts during "systole" - we pay attention to
heart size in both phases of cardiac function) had decreased from 4.7 to 4.0
cm, and the EPSS (our most objective echo indicator of pump function) had
decreased from 1.1 to 0.7. There was a "spangled" appearance to EN's
heart muscle - something we see on the echoes of patients with abnormally
thickened and stiff hearts.
 EN's 300 hour echo looked even better. Both systolic and diastolic
chamber dimensions had normalized, EN's ejection fraction was now increased,
and the "spangled" echo texture of EN's heart muscle was far less apparent - I
had never seen anything like this - hearts just don't decrease in size this
rapidly! I think that we are on to something when we combine MME with
metal detoxification, Bioresonance Therapy, and Stem Enhance. En is
going to continue his current nutritional and pharmacologic program, and he is
going to keep up with DMSA and Stem Enhance. I will see him again in
three months and repeat his echo. If heart function remains improved
then I will slowly cut back on his cardiac drugs. The changes in EN's
echo picture are highly significant to me as a Cardiologist.
EN's 300 hour echo looked even better. Both systolic and diastolic
chamber dimensions had normalized, EN's ejection fraction was now increased,
and the "spangled" echo texture of EN's heart muscle was far less apparent - I
had never seen anything like this - hearts just don't decrease in size this
rapidly! I think that we are on to something when we combine MME with
metal detoxification, Bioresonance Therapy, and Stem Enhance. En is
going to continue his current nutritional and pharmacologic program, and he is
going to keep up with DMSA and Stem Enhance. I will see him again in
three months and repeat his echo. If heart function remains improved
then I will slowly cut back on his cardiac drugs. The changes in EN's
echo picture are highly significant to me as a Cardiologist.
Helping a Runner to get Back on the Road - KD - 7/06
|
DATE |
EVENT |
| '01 | Initial sense of fatigue when running |
| 5/05 | Initial diagnosis of Dilated
Cardiomyopathy EKG - Atrial Fibrillation Echo - Dilated chambers (LVd 6.4, LVs 4.7 cm), at least mod. MR; EF 30-35% Perfusion scan - No ischemia, EF 30% |
| 5/05 | Triple challenge - Tin and Lead spills ® oral DMSA |
| 9/05 | Echo - (LVd 5.6, LVs 4.3 cm), EF 30-35%, mod to severe MR |
| 6/06 | Echo - (LVd 5.5, LVs 4.2 cm), EF 30-35%, MR 6 to 12 cm2 |
| 7/06 | MME and Stem Enhance begun |
| 8/06 | Echo - (LVd 5.4, LVs 3.7 cm), EF normal, MR 2 to 4 cm2 |
| ® | Continue Stem Enhance, DMSA, and repeat echo in 3 months |
KD has dilated cardiomyopathy, atrial fibrillation, and mitral regurgitation - and for no obvious reason, at least not one that cardiologists like myself are trained to recognize. KD should not have heart disease. KD is an addicted runner (like me); he watches his diet (we won't talk amount my diet), and he has followed a comprehensive nutritional program for years (better than mine). KD's blood pressure has never been elevated; he quit smoking 30 years ago, and he doesn't consume alcohol. So why is KD sick? My hypothesis is that KD's heart disease is due to heavy metal overload - so I treated him with DMSA and MME and he is getting better.
KD loves to run, but in 2001 he began to experience fatigue at speed and distances that were previously well tolerated. KD looks like a 50 year old, but he's really 64. Initially KD attributed this decline in running stamina to aging, but things got worse and KD sought medical attention in May of 2005. KD was in atrial fibrillation (uncoordinated rhythm where the atrial storage chambers beat rapidly and out of synchrony with the ventricular pumps, compromising overall cardiac performance). Cardiac echo demonstrated a dilated cardiomyopathy picture - all four chambers were enlarged, KD's ejection fraction was only 30-35%, and there was a mitral regurgitation signal involving 8 cm2 within the left atrium (we try to quantify the severity of mitral regurgitation (MR) by measuring its area on the echo study - this is not exact in a patient with atrial fib as the severity of the MR will vary with changes in the heart rate). A chemical stress perfusion study demonstrated no problems with KD's coronary artery blood supply. The diagnosis of dilated cardiomyopathy of unknown cause was made. Coumadin anticoagulation was initiated (patients with dilated hearts and atrial fib are prone to clot formation) along with Coreg as a beta-blocker (blocks the effects of adrenaline, which whips the hearts of cardiomyopathy and heart failure patients, hastening the loss of cardiac cells). KD continued to jog through all this, but noted fatigue from the Coreg - the most he could take was 12.5 mg/day (we usually recommend 50-75 mg).
It is my opinion that metal overload is the key cause of cardiomyopathy in the United States; chronic infection and inflammation may also play a role. KD has mercury amalgam fillings, several root canals, and dental abscess had been a problem in the past (and we know that toxicity in the mouth may lead to or become toxicity in the heart). A triple challenge study revealed not overly impressive spills of Lead and Tin, but we know that Tin may come out before Mercury ("hiding" the Mercury). We also understand that metal toxicity to the heart may be more qualitative than quantitative, related to sensitivities that may be both genetic and acquired (similar to how Autistic children are damaged by doses of Mercury that are apparently harmless to most kids). A program of oral DMSA chelation therapy was thus added to KD's medical and nutritional regimen.
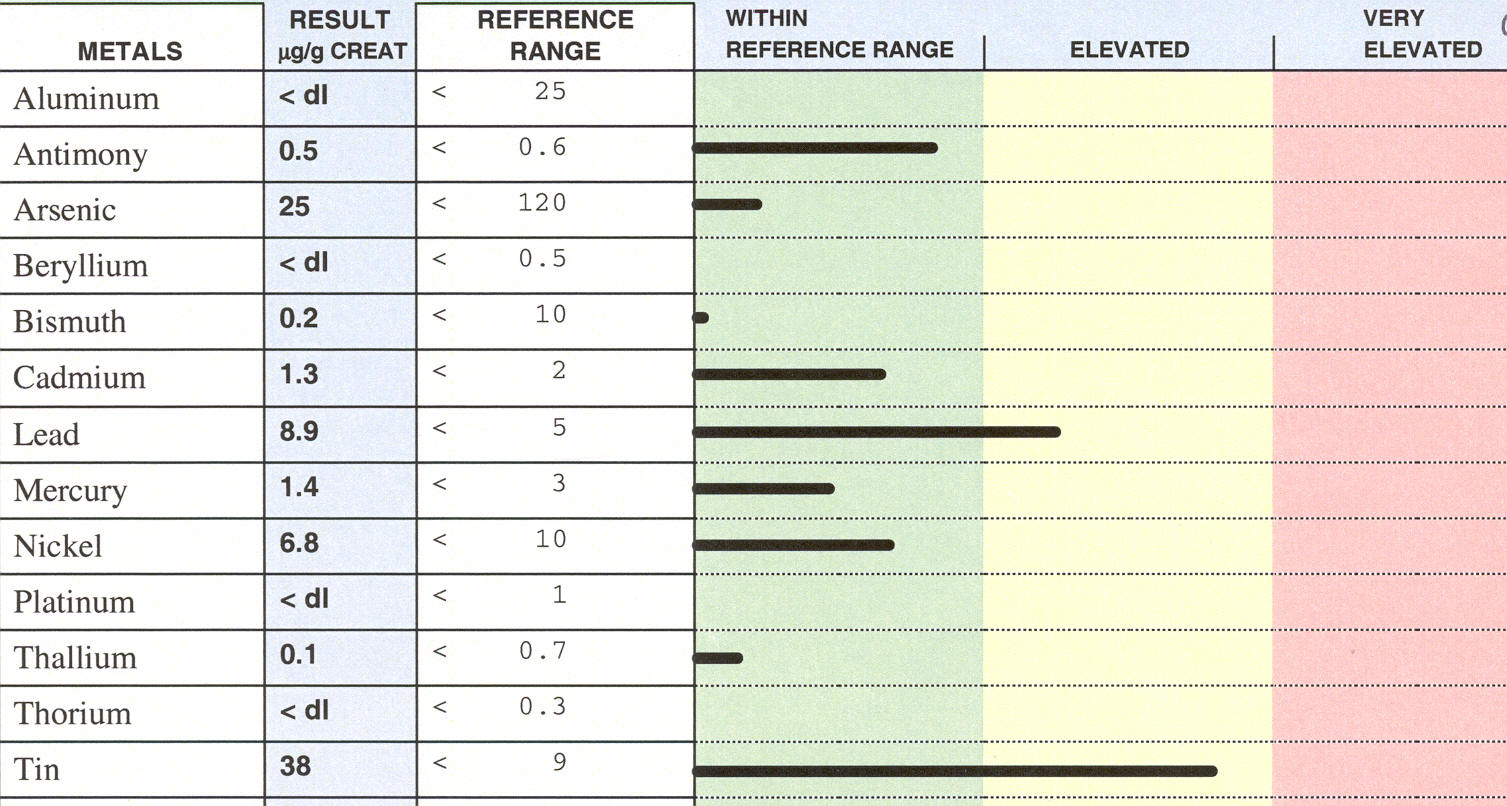
KD tolerated DMSA well. Six months later his echo looked better - the left ventricle was smaller, the diastolic (resting) size of his left ventricle had decreased from 6.4 to 5.6 cm (normal is 5.6 cm or less), and the systolic (contracting) dimension from 4.7 to 4.3). The EPSS, the most reproducible echo marker of pump performance, however, was unchanged at 1.4 (normal is £ 1.0 cm.), and KD's ejection fraction remained low at 30-35% (normal is 50%). KD kept up with DMSA based metal detoxification - his echo was repeated at the one year point (June '06), and further improvement was noted. The stage was now set for KD to undergo MME. DMSA had begun to remove metals from KD's heart (and elsewhere in his body). The next step was MME, aiming to drive more metal out of KD's heart and to improve cardiac function (we feel that MME increases intracellular energy production and stimulates proliferation of local stem cells - discussed elsewhere on this site). Stem Enhance (mobilizes uncommitted bone marrow stem cells out in to the circulation, from there to "land" in organs that need repair and regeneration) was begun concomitant to MME; DMSA and KD's nutritional program and Coreg were continued.
KD's echo picture improved markedly following 100 hours of MME. The left ventricular dimensions decreased a little more, but pump function improved a lot. KD's ejection fraction is now normal, as it the EPSS value. The degree of mitral regurgitation also lessened. Quantifying the severity of mitral regurgitation. is difficult in patients with atrial fibrillation, as the severity of valve leakage will vary with the heart rate, but comparing the echo images side by side I can see a clear change. The software on the echo machine allows me to planimeter (draw a circle around the MR signal to obtain a regurgitant area). Pre-MME the MR signal occupied 6-12 cm2, while post-MME the MR area was more in the 2-4 cm2 range. Again, quantification is difficult here, but the degree of mitral valve leakage had decreased, pump function had improved, and KD's heart had decreased further in size;
KD will continue with DMSA, and when he can scrape together some more time (KD has a lot going on and time is precious) he will receive another 100 hours of MME. As KD has been in atrial fibrillation for well over one year (and more likely 5 years) it is not likely that his rhythm will return to normal, so coumadin anticoagulation will be continued along with Coreg for its adrenaline blocking affects
Cardiomyopathy and Hypertension (Lead) with Atrial Fibrillation and Recent CVA - DF - 11/06
|
DATE |
EVENT |
| '02 | Left ventricular dilated - LVd 6.0 cm. |
| 10/05 | Four chamber cardiac
enlargement - LVd 6.0. Triple challenge with a predominate Lead spill |
| 3/06 | LVd 5.8 with a normal ejection fraction |
| 10/06 | Atrial fibrillation with an
embolic stroke LDd 6.3 with an ejection fraction of 40% |
| 11/06 |
300 hours MME with DMSA and Stem Enhance LVd 5.7 with a normal ejection fraction |
| 1/07 |
Chest discomfort and recurrent atrial fibrillation Minimal coronary disease by angiography - LVd 5.9 with an ejection fraction of 45% |
| 2/07 | Back in normal rhythm with LVd 5.8 and a normal ejection fraction |
DF presents with the triad of hypertension, cardiomyopathy, and atrial
fibrillation - all three, in my opinion, due to or aggravated by Lead.
All three conditions, to my analysis, seem to be improving with the addition
of MME based Lead detoxification to standard drug and nutritional therapy.
DF has been troubled by high blood pressure for at least a decade; drug
therapy was not well tolerated and his left ventricle was seen to be dilated
at 6.0 cm. in 2002 (normal is ≤ 5.6 cm.). DF and I began working
together in 10/05. His echo showed four chamber cardiac enlargement and
just preserved systolic function. A triple challenge study revealed a
predominate Lead spill. Drug, nutritional, and homeopathic measures were
utilized (formal Lead detoxification was not initiated due its cost) and DF
did well, with a normalization of his BP an a decrease in left ventricular
chamber diameter to 5.8.
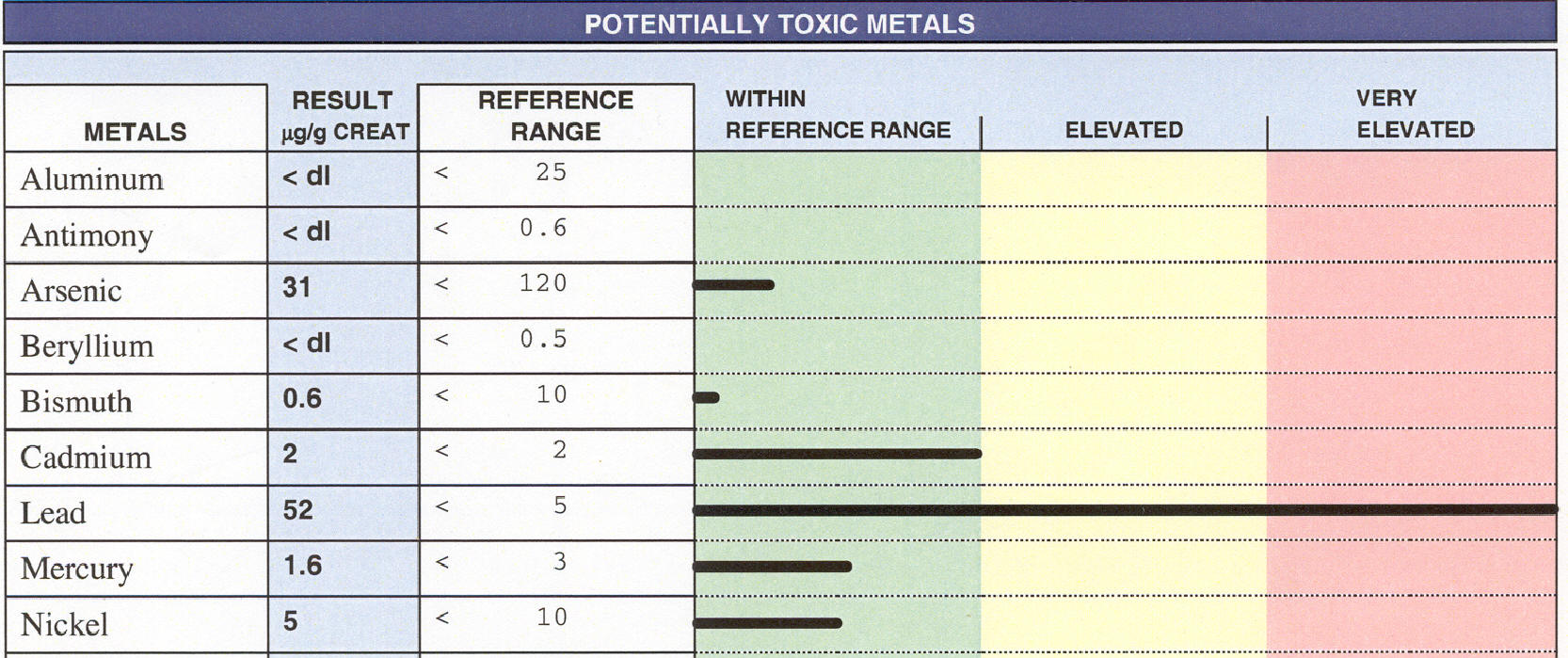
DF's condition worsened abruptly in 10/06. He developed atrial fibrillation, an irregular cardiac rhythm that cancels out the pump priming function of atrial contraction. Pump function deteriorated, and it deteriorated markedly - DF's ejection fraction fell from normal (50-55%) into the 35-45% range, and his left ventricle dilated up to 6.3 cm. DF sustained a stroke, not on the basis of hypertension or impaired blood flow to the brain, but rather due to mobilization of a blood clot from the left atrium to the brain. In atrial fibrillation, the atria no longer contract rhythmically and in synchrony with the ventricular pump, and for this reason cardiac output falls and the ejection fraction may decrease (as it did in DF's case). The atria instead beat lack a sack of worms; blood flow is stagnant and small clots can develop within the atria. Here they do no harm, but if they break off and travel to a distant location (we call this embolization), they can cause a stroke, a heart attack, gangrene, or kidney failure, depending upon where they land. For this reason we recommend anticoagulation, typically with Coumadin, to patients in atrial fib. The problem here was that DF did not realize that he was in atrial fibrillation. This arrhythmia had developed since his last office visit two months earlier; he thus wasn't on a blood thinner, and the result was an embolic stroke.
Post-stroke we placed DF on coumadin anticoagulation, and then set out to address his underlying cardiomyopathy. DF received 300 hours of MME, combined with oral DMSA as a Lead chelator. DF's rhythm had reverted to normal even before we began him on MME, but his heart rate was quite low, limiting Beta-Blocker therapy and precluding the addition of an anti-arrhythmic agent to DF's program. DF cruised through MME. DF's post-MME echo demonstrated normal pump function and a left ventricular dimension of 5.8 cm. DF kept up with oral DMSA but did not utilize a magnetic sleep pad. Drug and nutritional therapies were all continued.
DF experienced chest discomfort in 1/07. I had attributed DF's pump dysfunction to cardiomyopathy, but with this new complaint of chest discomfort, I became concerned that DF might also have coronary disease. angiography was carried out, and demonstrated a 60% narrowing only in the diagonal branch of the LAD - the major vessels wee all normal in appearance. the surprise was that DF was back in atrial fib, and he didn't know it. Pump function had fallen again, just as it had when DF went into atrial fib the first time. Coumadin anticoagulation was resumed, and I added Zeolite as a metal chelator as well as Asyra based homeopathic therapy to DF/'s program - DF converted back into normal rhythm, and again pump function normalized.
DF's current program will be continued. His heart rate is too low for formal anti-atrial fib drug therapy. If a pacemaker was placed, then I could address DF's rhythm issue more aggressively, but DF does not want to take this step (which would preclude future MME). Throughout this process DF's strength and speech deficit due to his 10/06 stroke have slowly but steadily lessened; some of this is due to the normal recovery process and some may be due to scatter of some of the MME energy to DF's brain. Coumadin anticoagulation will be continued for at least six months or until we are convinced that atrial fib will not recur, and I will watch DF closely over this time period.
Congenital Heart Disease with Hypertensive Heart Disease in and Adult - SH - 7/05
SH presented in mid-'03 with congestive heart failure, with two distinct causes. Formerly active and on the go, this 66 year old college professor had been slowing down over the preceding two years; now she couldn't even climb a flight of stairs without loosing her breath. SH had been hospitalized with Rheumatic Fever as a child, and in 1958, well before the first echo machine had been invented, a physician diagnosed the presence of Mitral Valve Prolapse based upon physical exam. SH required no treatment and her subsequent health has been excellent. She watches her diet, takes a good program of nutritional supplements, and really hasn't required much in the way of medical care.
When I saw SH for the first time in mid-'03, she did need some assistance. Her BP was 160/120, with a heart rate of 100. Her EKG was markedly abnormal, and her echo surprised me. The left side of SH's heart was hypertrophied (abnormally thickened heart muscle), a consequence of hypertension. Her left heart was stiff, and it also wasn't pumping well, with an ejection fraction of 35-40% (percentage of blood ejected with each beat - normal is 50-55%). This I expected, on the basis of SH's high blood pressure, but what I didn't expect was the marked enlargement, hypertrophy, and pumping dysfunction of SH's right heart. This wasn't due to high blood pressure or childhood Rheumatic Fever, but rather to the life-long effects of Partial Anomalous Pulmonary Venous Drainage, a congenital heart defect. Here a vein that is supposed to channel oxygenated blood from the lungs to the left heart is attached instead to the right heart. Blood is pumped from the right heart to the lungs; some then drains into the left heart, from where it is pumped out to the body, but some returns to the right heart, from where it has to be re-pumped back to the lungs. This cycle repeats itself, straining the right heart. Early on, the right heart chambers can dilate to increase their pumping efficiency, but over time the right heart begins to thicken and fibrose. The pressure in the right heart begins to rise, further increasing the right hearts workload - then it begins to fail.
If detected early in life (easy to do today with the echo machines of today), these "shunt lesions" are corrected surgically. When seen in a 66 year-old with heart failure, the time frame for surgical correction has passed - the situation is too-far-gone for surgical relief. Realizing that I couldn't fix SH's right heart, I did what I could for her left heart. A drug and nutritional program aiming to improve pump function and lower BP was initiated, and within six months SH's left heart ejection fraction was back to normal. Early on SH experienced some side effects from her BP meds, but with a little adjustment we were able to arrive upon a regimen that SH could live with. On this regimen SH was living better. She was back in the classroom and able to carry out necessary activities - but desired activities and exercise left her winded and fatigued.
A packed red cell study demonstrated the presence of Cadmium, Lead, and Mercury in SH's system, not a surprise given her high blood pressure. We knew that MME could not reroute the piping in SH's heart, but I felt that it just might strengthen the chronically strained muscle cells in SH's right heart, "turning back the clock" a little with respect to the progressive right heart damage occurring on the basis of the congenital shunt lesion. I did feel that MME would be of value to SH's left heart, strained by run-of-the-mill hypertensive heart disease. It appears that I was right.
SH received 300 hours of MME during the summer of "05. Post-MME her right heart doesn't look any different by echo assessment, and I didn't think that it would, but SH's overall cardiac performance has certainly improved. SH can do more, including riding her bike and walking at a brisk pace. Her recovery time following activity that does produce fatigue has decreased. She feels lighter on her feet, like she has "styrofoam" in her chest, instead of "sandbags". Classes start in the fall and SH is looking forward to teaching them. She rates herself as 50% better; in her own words - "I feel more energetic and am walking farther each day without breathing stress. I also can enjoy some bike riding again. I feel my nerves are calmer than before the MME experience. I feel I'm growing stronger each day and sleep more soundly at night. I am grateful for the opportunity to obtain MME treatments". SH received DMSA during MME, to help remove toxic metals from her body; post-MME she will sleep on a negative field only sleep pad and take DMSA on a periodic basis, to continue this process. SH's BP had come under good control with medical/nutritional therapy, but now its down to 110/70 - fantastic. Of interest, the presence of a diagonal creases on one's earlobes is associated with heart disease. No one can explain why, but the association exists. SH had prominent earlobe diagonal creases before beginning MME - now they are less apparent. I can't explain this, but view this change as a positive sign.
7/06 Update - SH continues to do well on all cardiovascular fronts, essentially without any limiting symptoms. SH remains intellectually active as well, writing, participating in many seminars and learning activities, and she continues to teach at the College level
Sick Sinus Syndrome - Don't Stop Until the Job is Done - RH - 3/05
We learn from our patients in Medicine. RH's case reminded me of a rule that had been drilled into me long ago - that its not a good idea to stop a successful therapy until the job is done. RH had been troubled by cardiac arrhythmia for years. She had tachy-brady syndrome. In seniors, and RH is 81, this condition is often described as sick sinus syndrome (referring to dysfunction of the pacemaker center, the sinus node). RH would experience episodes of rapid heart rate, followed by episodes of an abnormally slow rate, an up and down, hectic pulse. Drug treatment here is difficult, in that the medications used to slow the episodes of tachycardia (fast rate) could bring on or worsen the episodes of bradycardia (low heart rate). Medical treatment is thus a balancing act. Sometimes we get the drugs, and their doses, right; other times we must resort to pacemaker implantation. With a pacemaker in place we can advance the drug doses as required to address the tachycardia, without fear of producing symptomatic bradycardia. I had discussed these options with RH on many occasions, but RH didn't want a pacemaker, and RH wanted to avoid drug therapy if at all possible - she had always reacted poorly to prescription therapy. We argued these issues on many occasions, and RH always won - after all, its her body and its her health, not mine.
There was really no reason for RH to have a cardiac arrhythmia, nor was there a specific reason for RH to be so sensitive to drug therapy. She didn't smoke, her blood sugar was normal, and she followed a good diet; she wouldn't let me carry out a stress test but she had never experienced chest pain suggestive of coronary disease. When things don't make sense, when patients present with disease states they shouldn't have, I think of toxicity, especially heavy metal toxicity. HR's Mercury amalgam fillings had been removed years earlier, but a challenge study carried out in 2000 revealed a moderate urine Mercury spill, indicating the presence of Mercury in her tissues.
HR took several courses of moderate dose oral DMSA; with this her rhythm symptoms didn't resolve, but they did quiet down. We observed that HR's MCV, a component of her CBC (complete blood count) could be used a biomarker of her toxicity status. Her MCV (mean corpuscular volume) was abnormally high, indicating that HR's red blood cells were abnormally large. Low thyroid status and B12 deficiency are associated with an increased MCV, but these were not issues with HR. The thinking here is that Mercury and other toxins interferes with the production of Hemoglobin and other components of the red cells, causing them to vary in size and be abnormally large. With DMSA therapy in 2000, HR's MCV fell from 105 to 96.9 (normal is < 101). HR's sensitivity to prescription medications might also be related to metal overload. If the enzymes responsible for drug metabolism and detoxification are poisoned by Mercury, it makes sense that she would be sensitive to them. Getting HR to take DMSA, or any other drug for that matter, was a challenge. She didn't want to take DMSA long term. The only drug she would take for her heart was Digoxin,. HR took Digoxin, and an extensive nutritional program, and this kept HR out of trouble - for a while.
HR's symptoms worsened in late '04. A heart rate of 55 precluded additional drug therapy (which she would not have taken), so again I brought up the idea of pacemaker implantation. HR was not enthusiastic. I knew that tissue Mercury was still on board, and HR's MCV had risen slightly to 99.7. HR began a program of DMSA 500 mg every other evening, while sleeping on a 10 Gauss negative field only pad. Two months later she received 152 hours of MME. This program worked. Hr's sensation of palpitations improved considerably. An EKG obtained in the office showed a heart rate of 68. A 24 hour EKG monitor demonstrated an average heart rate of 45 (her heart rate would slow down at night), but only 9 premature atrial beats were observed. HR's MCV decreased to 95.5. HR was feeling better and I was pleased.
Our plan was for HR to continue to sleep on the magnetic sleep pad, and to keep up with DMSA therapy, as I was under no illusion that all the Mercury in her body had been eliminated. Two months out from MME, HR was to stop Digoxin therapy and then undergo a treadmill stress test. HR decided not to undergo the stress test. She ran out of DMSA, and did not order more. Digoxin was continued. She returned in mid-'05 with palpitations and a heart rate of only 42. Her MCV was back up to 101. Digoxin was stopped and HR's rate rose to 68, but then she developed atrial fibrillation, a hectic, uncoordinated rhythm, thankfully with a controlled rate. Signs of right sided heart failure developed. There were no findings on non-invasive testing to indicate a blood clot or pneumonia, conditions that might strain the right side of HR's heart. I was stuck as to what was going on, and urged HR into letting me carry out a heart catheterization. This revealed totally normal coronary arteries, brisk left heart pumping function, but a moderate elevation in HR's right heart pressures was observed, along with a low blood oxygen saturation.
What was going on here? First, HR had something going on in her lungs, as well as in her heart's electrical system; she will see a lung specialist in the non-to-distant future. Second, and this is an important point to any patient undergoing MME or a program of metal detoxification, not staying on DMSA was a mistake. We are not going to remove all the metal from your heart, or your other internal organs, with just two months of sleep pad therapy and 152 hours of MME to your heart. It takes decades for the metals to accumulate to the point where they bring on overt illness. It makes sense that it will take months, maybe years, to control or reverse the situation with a program of metal detoxification, no matter how powerful the program might be. In retrospect, staying on the sleep pad, but not taking DMSA, might have allowed for metals to be mobilized from HR's internal organs, but not rapidly excreted from her body. It may be that some of the metal landed in HR's heart (post-MME we feel that the Mercury concentration in HR's heart was lower than in her other organs, so maybe Mercury redistributed from the liver and kidneys, etc., to HR's heart - this is a theory and I can't prove it, but it makes sense).
10/05 Update - DMSA was resumed in 7/05, following HR's cardiac catheterization. By the time she got in to see the pulmonary physician, HR was feeling better. HR's chest CT scan was non-revealing, and the pulmonary physician who evaluated HR did not feel that any active lung disease was present. When I saw HR again in 10/05, she was feeling much better. Palpitations, HR's primary symptom, had resolved, and her EKG demonstrated a return to normal rhythm. Carpal tunnel syndrome wrist pain, and a hoarse voice, issues in mid-'05 when HR was in atrial fibrillation and feeling poorly, also had resolved. On physical exam, I could no longer detect findings of heart failure. Her BP was 120/70, notable in that HR's systolic blood pressure had always been in the 100-110 range, associated with dizziness.
Now, why did HR improve with sleep pad + MME + DMSA therapy, then fall apart, with multiple symptoms related to multiple organ systems (atrial fibrillation, heart failure, pulmonary hypertension, carpal tunnel, hoarse voice, generalized malaise), when she was temporarily off DMSA, and then improve markedly when DMSA was resumed? I think that HR's temporary, mid-'05 symptoms were related to Mercury release from her internal organs (the sleep pad mobilizes the metals) without DMSA to shepherd the metals out of her body. I think that HR's chronically low blood pressure was related to dysfunction of her autonomic nervous system due to Mercury toxicity. Our plan will to keep HR on metal detoxification therapy. At this point we will switch from DMSA to low dose topical DMPS, which seems to be more effective than DMSA in cardiac patients, and keep this therapy on board at a low level for one to two years.
Carotid Disease, Non-dilatable Coronary Blockages, and SAD - BR - 11/05
|
|
EVENT |
| '03 | New onset angina - Angiography shows non-dilatable diagonal narrowing |
| 10/04 | Normal 6:27 stress perfusion study |
| 7/05 |
Recurrent angina despite drug therapy:
· Abnormal 7:00 stress echo study · Abnormal triple challenge study · Carotid ultrasound with 70% Left Internal Carotid Artery narrowing |
| 8/05 | Negative field only sleep pad
with topical DMPS-Glutathione initiated 35 hours EECP ® Angina improved |
| 10/05 | 100 hours MME to her head, with ongoing metal detoxification, sleep pad and Bioresonance therapy ® Angina and SAD resolved; carotid ultrasound improved. |
This 69 year-old non-diabetic female non-smoker with medically addressed hypertension and hyperlipidemia presented in '03 with new onset chest pain. Angiography revealed a non-dilatable narrowing in the diagonal branch of the Left Anterior Descending coronary artery. Beta blocker therapy was poorly tolerated, greatly aggravating a pre-existent problem with seasonal depression. BR was switched to a calcium channel blocker, with satisfactory results, and a normal 6:26 nuclear stress study in the fall of "04. Angina recurred in mid'05. Two mm of ST depression was brought out on BR's 7/05 stress echo study. A high-pitched sound (carotid bruit) was heard over the left side of BR's neck, and ultrasound demonstrated the presence of a 70% Left Internal Carotid Artery narrowing. BR did not wish to be considered for carotid artery surgery, and I knew that a coronary study would show the non-dilatable Diagonal narrowing, so we decided to pursue a non-invasive approach to BR's combined carotid and coronary disease.
Fish oil, Arginine, Co-Enzyme Q, Ribose, and Magnesium were added to BR's already comprehensive supplement program. 35 hours of EECP were carried out, and with this BR's angina improved. A triple challenge revealed spills of Cadmium, Lead, and Mercury; we addressed this with topical DMPS-Glutathione, applied in the evening with BR sleeping on a negative field only magnetic sleep pad. BR has been troubled with Seasonal Affective Disorder (SAD). Every fall and winter, her mood would fall, requiring therapy with the anti-depressant Paxil. BR wanted off Paxil and she really wanted to get rid of the SAD so we treated her with 100 hours of MME to her head in 10/05. Bioresonance therapy was initiated soon thereafter and BR's other treatments were continued.
BR improved on multiple fronts with this multi-modality program. On her own BR stopped two cardiac drugs. BR's blood pressure fell (an expected and not unwelcome effect), so I had to decrease her anti-hypertensive agent by 50%. Angina has all but resolved. BR is feeling better overall, with increased energy. BR was able to stop Paxil and this winter her mood remained upbeat and bright - so long SAD.
EECP was carried out to improve BR's coronary status, with MME to the head to
fix BR's mood, but all of these treatments improve cardiovascular function in
general, and there was certainly some scatter of the
magnetic affect to the region of BR's carotid arteries. We repeated BR's carotid
ultrasound in early '06 - and what do you know - it looked better (see
graphics below). This finding, an anatomic regression of
atherosclerosis, delighted us, but it really it should not have surprised us,
as a number of European studies have demonstrated an improvement in
cerebrovascular blood flow and function following static magnetic field
treatment. 
The tighter the carotid narrowing, the greater will be the velocity of blood flow within the narrowed vessel (think of your thumb over the garden hose). The reduction in Left Internal Carotid Artery velocity from 265 to 214 cm/sec. is significant and important. The velocity increase in the less severely diseased Right Internal Carotid Artery velocity from 87 to 103 is within measurement error is not physiologically meaningful.
The Internal Carotid Artery, which serves the front of the brain, arises from the Common Carotid Artery in the neck. Another measure of Internal Carotid disease severity is the velocity ratio between the Common and Internal Carotid on the same side. In BR's case the ratio fell significantly on the left and rose only minimally on the right.
Atrial Fibrillation and Single Vessel Occlusive Coronary Artery Disease - MG - 7/06
MG experienced a prolonged episode of chest pain 20 years. Less severe and less prolonged chest tightness followed, prompting her to seek medical attention. A stress thallium scan (a brand new diagnostic study at that time) returned normal, indicating that MG was not at risk for a heart attack. MG's symptoms waxed and waned over the years, but didn't really interfere with her activity level or enjoyment of life. Stress tests were done intermittently and returned benign. She was hospitalized three years ago for a somewhat different pain, and was found to have gastric inflammation related to the use of Advil for arthritis pain.
I began working with MG early '06. MG's chest pain was coronary in quality, but her 3:13 stress echo study looked good - I could see no evidence of coronary insufficiency. We began a program of risk factor reduction, with ongoing medical therapy for MG's hypertension.
MG came in in early 5/06 with chest pain and shortness of breath. Her EKG demonstrated Atrial Fibrillation with an initial heart rate of 150. Digoxin and Metoprolol (a Beta blocker) were added for heart rate and angina control. Angiography revealed chronic occlusion of MG's Right Coronary Artery, with well developed left to right collateral flow, totally normal appearing Left Anterior Descending and Circumflex systems, and brisk pump function. MG's RCA may have closed 20 years ago, but she had built up natural bypasses, such that the blood supply to her RCA was good enough to hide the problem on her stress echo and stress nuclear scans, but not good enough to keep her pain free and in rhythm.
Coumadin anticoagulation was initiated to prevent the formation of blood clots within MG's now fibrillating atria. MG's heart rate was brought down into the normal range with medical therapy, but she was still experiencing chest pain, as well as fatigue from her medications. MG was not enthusiastic regarding electrical cardioversion, so we began her on a program of MME and Amiodarone, our most effective anti-arrhythmic agent. A challenge study demonstrated spills of Mercury, Lead, Cadmium, Antimony, and Aluminum, so MG took DMSA concomitant to her MME sessions, aiming to clear these toxins from her heart. MG did not convert back to normal rhythm during MME, but four weeks later she did, and then she felt great. Metoprolol was phased out, the doses of Digoxin and Amiodarone were decreased, and aspirin was substituted for Coumadin. Metal detoxification utilizing the combination of DMSA and Zeolite will be continued, and MG's challenge study will be repeated in the future, to guide her metal detoxification program. In retrospect, MG was troubled by an abscessed tooth around the time that she went into Atrial fib -it just might be that bacteremia and inflammation related to this dental issue precipitated the onset of arrhythmia. In any event, MG is back in normal rhythm, she feels great, and we have her on a comprehensive program of nutritional, detoxification, and limited drug therapy, and I think that her outlook is quite good.
AMRI of NW Ohio provides MME treatment under the guidelines of an Investigational Review Board, consistent with FDA regulations.
Please note that MME treatment is considered to be experimental by the FDA. Although many patients have improved, no guarantee of success is implied.