
Link to IMT DVD - Part Two Carotid Intima-Media Thickness Assessment

A New Window into the Heart and Cardiovascular Circulation
Physiology and anatomy interface at the inner (intima-media) thickness of our great vessels. It is within the intima-media that abnormalities in vascular biochemistry layer out soft, vulnerable plaque. It is within the IMT that vascular disease first progresses and it is within the IMT that vascular disease first regresses. The IMT is the leading edge of cardiovascular disease. CIMT measurement allows us to quantify, and then follow, your overall plaque generating status in a manner that is non-invasive, quantitative, and reproducible. CIMT is moderate in price and does not expose you to ionizing radiation. We will use CIMT to determine risk, guide our preventive efforts, and then gauge the effectiveness of these maneuvers, with greater precision than our current best methods can provide.
Clinical
Cardiology, the discipline in which I was trained, focuses on “flow-limiting”,
“surgical disease”, 70-90% barrowings that compromise flow to the heart with
exercise. We diagnose these “lesions” when exercise/chemical stress EKG, echo,
or nuclear studies demonstrate “flow disparity” between “diseased” and normal
vessels, or “ischemia” (impaired cardiac energy production due to insufficient
supply of oxygenated blood). We address these focal lesions by rendering blood
flow sufficient, either with bypass surgery or stent placement. If
revascularization is not possible we will carry out EECP to generate a
collateral circulation, or we might prescribe drug therapy to lower your HR and
BP, to decrease your heart’s requirement for oxygenated blood (if we can’t
increase supply then we must decrease demand). Following revascularization
blood flow is restored, your symptoms resolve, and your stress studies
normalize. Revascularization can prevent a heart attack (or stroke when lesions
compromise blood flow to the brain) and save your life – but it doesn’t prevent
most heart attacks, strokes, and cardiovascular deaths, as
the initial manifestation of vascular disease in 50% of afflicted
Americans is sudden death!
That’s right; these people never knew what hit them. Many had no symptoms, most did not have flow-limiting narrowings, and some had recently passed a stress test. They didn’t die because a 90% narrowing closed off (when a 90% narrowing closes you typically experience a small heart attack or none at all as a protective collateral circulation has formed). You die of a heart attack when a 30-60%, “non-surgical” narrowing closes off abruptly – there is no pre-existent collateral protection and an entire wall of the heart is lost. The same principle holds true within the cerebral circulation – only 10% of strokes are due to closure of a vessel with a high-grade narrowing. The rest of our strokes and heart attacks occur when the immature or “vulnerable” plaque within a non-flow restrictive narrowing cracks, spasms, or clots. Relying of the presence of symptoms or an abnormal stress test to protect you from cardiovascular calamity, to prompt you and your doctor to take pre-emptive or corrective action, will likely be a failed policy – as Clinical Cardiologists we would not even have seen you.
OK; we all know this, and that is why we practice Preventive Cardiology. Let’s work on your risk factors before you develop your first “lesion”. Sounds sensible, but who are we to treat with prevention – all 240 million of us? At what age should we start? How aggressive should we be? Should we put asymptomatic 30 years-olds on a statin? We should if they have early disease, a high CRP, and oxidative stress. But if their vasculature is pristine and no other risk factors are present, if they really aren’t at any risk, and we then begin them on life-long therapy with potent drugs, then we are going to hurt a lot of people to prevent heart disease in just a few, and we are going to spend a lot of money. Knowing when to prevent and how hard to prevent is a challenge to Preventive Cardiology and to the resources of our society. Also difficult is determining whether a specific preventive measure is successful or not in a given individual. If we focus only on cholesterol – well, 50% of heart attack victims have normal cholesterol, so cholesterol reduction is not the magic answer. What we need is a risk-free, reproducible, quantifiable measure of your “plaque status” that can be repeated over time to tell whether your plaque volume is receding or progressing, whether your preventive program is succeeding or failing.
CIMT is this measure.
CIMT measures, in micrometers, the thickness of the inner wall of your carotid artery, the intima (the endothelial cells that line the artery and soft plaque that is accumulating within and behind it), and the media (the smooth muscle layer of the vessel). The intima-media segment of a vessel (IMT) is the interface between physiology and anatomy. An abnormal IMT is the site of soft plaque (and soft plaque tends to be vulnerable plaque) accumulation and it is associated with endothelial dysfunction (inability of the endothelial cells to make protective nitric oxide). We know what the average CIMT value is for a man or women of your age, for smokers and for non-smokers, for diabetics and non-diabetics, etc. If your CIMT is significantly above average for your age and gender, then you are in some trouble. CIMT progresses in the average American at a rate of 0.014 mm/year. If your IMT is progressing faster, than you are depositing soft plaque in all of your arteries at an above average rate; you are now in big trouble and you are at increased risk of heart attack or stroke. Conversely, if our preventive efforts stabilizes or regress your CIMT value (yes – here we are melting away soft plaque) then your risk of an adverse event is minimal. We can lower cholesterol and BP with drugs, but this doesn’t guarantee that we are regressing or stabilizing plaque, but if we regress your CIMT, we confirm that our preventive efforts are really working.
Which sound better to you – cholesterol control or plaque control?
Conversely, if your CIMT is progressing rapidly despite control of your standard risk factors, then we must look deeper into the potential causes of atherosclerosis that you might bear.
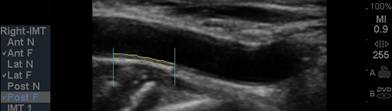
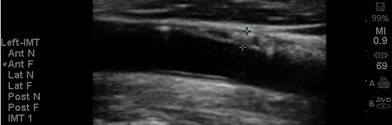
The CIMT procedure is
simple. An ultrasound study is carried out of the carotid arteries in your
neck. A specialized software program is used to precisely measure the mean and
maximum IMT. Standard carotid ultrasound is looking for “flow-limiting”
stenoses, narrowings that could be addressed surgically. This is not what we
are interested in with CIMT testing - we will be measuring soft plaque
accumulation in non-overtly diseased vessel segments (if plaque is identified we
measure the CIMT at an adjacent, normal appearing segment). While the presence
of plaque obviously has significance, it is the IMT parameter that best predicts
the presence and severity of atherosclerotic vascular disease elsewhere in your
body, it’s risk of progression, and your risk of sustaining an atherosclerotic
event (think of IMT as the “staging ground” for obstructive plaque – the higher
the IMT, the greater the rate of IMT progression, the more rapidly will large,
obstructive plaques form). Over 2,000 studies (go to www.pubmed.gov and enter
Carotid IMT) document the link between CIMT and current risk, and an even more
powerful relationship between the rate of change in CIMT and future risk. We
will use CIMT to help us decide who should be treated with preventive measures
and how aggressive our efforts should be. We will use the rate of change of
CIMT to gauge the success of the regimens that we construct for you.
CIMT allows us to “keep score”.
The tables below list factors that have been associated with an increased CIMT and/or an increased rate of CIMT progression, as well as therapies that have been shown to delay or prevent CIMT progression.
|
Factors associated with Increased CIMT and/or Rate of CIMT Progression |
|||
|
High LDL |
Oxidized LDL |
Low HDL |
High Triglycerides |
|
Lipoprotein (a) |
Hypertension |
Smoking |
Diabetes |
|
Mercury |
Arsenic |
Low Antioxidant Defense Level |
|
|
Overweight |
Homocysteine |
Insulin Insensitivity |
Low Vitamin D |
|
Oxidative Stress |
Infectious Burden |
Sleep Apnea |
Hypothyroid |
|
Low Selenium |
Low Magnesium |
High Fibrinogen |
Kidney Failure |
|
High Stress |
Depression |
Family Hy of CHD |
Standing at Work |
|
Low Testosterone +/- High Estradiol in Men |
Periodontal Disease |
ADMA |
|
|
Inflammation |
Air Pollution |
Allergy and Asthma |
|
|
Therapies associated with Delay or Prevention of CIMT Progression and/or CIMT Regression |
|||
|
Lipid Reduction |
Statins |
Niacin |
Fibrates |
|
Sugar Control with Metformin and Actos (but not with Sulfonylurea agents) |
|||
|
Estradiol in Women |
Tamoxifen in Women |
Smoking Cessation |
Probucol |
|
Thyroid Hormone |
Antioxidants |
Pomegranate Juice |
GliSODin |
|
Fish Oil |
Colestipol + Niacin |
Metoprolol |
Calorie Restriction |
|
Quinapril |
|
|
|
We will be adding to these tables as more research comes out. We are currently evaluating the interaction between metal detoxification, reverse cholesterol transport with unsaturated Phosphatidylcholine, and static magnetic field therapy on CIMT and other measures of disease activity in stable angina patients.
The cost of CIMT is $200. While the value, and incremental value of CIMT above and beyond risk factor analysis has been conclusively demonstrated, neither Medicare nor the major commercial insurers in NW Ohio will cover the cost of CIMT (but not to worry, they will be happy to cover the cost of your heart attack, stent, bypass surgery, and cardiac transplantation that maybe we could have prevented). They consider CIMT to be a “screening procedure” or “experimental”. The 2,000 published studies on IMT testing are not enough. Until the position of Medicare changes, the cost of CIMT will be your responsibility. We can give you a receipt and you can turn it in to your insurer, but we will not write your insurer to request preauthorization (this never works and serves only to waste our time and your time).
We have already found undiagnosed, “surgical” narrowings during IMT testing of “normal” individuals. If potentially obstructive plaque is identified, we will refer you for a formal carotid ultrasound, which involves blood flow velocity measurement to quantify the degree of vessel stenosis.
We are the only practice in NW Ohio to offer CIMT testing, so your personal physician and family members may not be aware of its value. We are currently working on a DVD presentation covering CIMT (and brachial artery flow-mediated vasodilation, a direct measure of endothelial function).
![]()
![]()


![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
Interpreting
Your CIMT Findings
(Handout you receive along with your CIMT report)
In individuals not known to have CV disease; CIMT testing is done to assess risk for CV disease and CV events. In patients with known vascular disease, the current CIMT reflects your current plaque producing potential. It serves as a baseline, such that future measurements can tell us whether the underlying plaque generating process has been stabilized or whether it is still progressing.
If you do not have known CV disease, we can use your CIMT (adjusted for age bracket), to predict your risk, and to help us decide whether you need preventive efforts, or how aggressive we should be. For example, if you are 45 years of age and have a CIMT at the 90th percentile for this age bracket, you have more soft plaque than do 90% of our colleagues; you are at risk for CV disease and CV events and we need to get to work. Conversely, if you are 65 years of age and have a CIMT at the 10% percentile (for age) and no visible plaque, then you are probably home free as far as CV disease is concerned. If we are treating you to decrease your CV risk, I will emphasize measures that have been shown to decrease or stabilize IMT, as measures that favorably affect CIMT also decrease event rates (for example, if your sugar is high and we treat you with Metformin, we will lower your sugar, favorably affect the CIMT, and lower your event risk; if we use a Sulfonylurea drug, we will lower your sugar, but we will not favorably affect your CIMT, nor will we decrease your event risk). We can repeat your CIMT periodically, probably once a year (many therapies will affect the CIMT within 6 months). If the CIMT is stable, your current program will be continued; if it is still progressing, then we need to work harder.
Reference group data is attached. The top page contains mean CIMT values obtained from Brits who are ultra healthy or who have one or more risk factors. The second page contains the ARIC (Atherosclerosis Risk in Communities) data describing mean and percentile CIMT findings recorded in 5,000 45-65 year old Americans. Population values pertaining to young people and more senior Americans is not as firm.
If your
CIMT study demonstrates large, potentially obstructive plaque, then we will
recommend a formal ultrasound, which includes blood flow velocity measurement to
better quantify the narrowing.
At your next visit I will discuss with you your IMT value, in relation to your
age bracket and current health status. If appropriate, we will take a more
aggressive aim at your risk factors or possibly initiate a program of
anti-atherosclerotic therapy – but now we know what we are treating – not
numbers but plaque buildup and plaque building potential, and now we have a real
measuring stick, future CIMT determinations.
IMT DVD Bibliography
Normal (Population Expected) Values:
Normal Value of Carotid Intima-Media Thickness-A Surrogate Marker of
Atherosclerosis: quantitative Assessment by B-Mode Ultrasound
Lim, TK, et al. Journal of the American society of Echocardiography Feb. 2008
p112-116
Carotid Artery Intimal-Media Thickness Distribution in General Populations As
Evaluated by B-Mode Ultrasound
Howard, G, et al. Stroke 1993;24:1297-1304.
Distribution and Cross-Sectional Age-Related Increases of Carotid Artery Intima-Media
thickness in Young Adults: The Bogalusa Heart Study
Stein, JH, et al. Stroke 2004;35:2782-2787.
Cardiovascular Risk Factors and Increased Carotid Intima-Media Thickness in
Healthy Young Adults – The Atherosclerosis risk in Young Adults (ARYA) Study
Oren, A, et al. Arch. Intern Med. 2003;163:1787-1792.
Carotid Intimal-Media Thickness Is Related to Cardiovascular Risk Factors
Measured From Childhood Through Middle Age – the Muscatine Study
Carotid intima-media thickness by B-mode ultrasound as surrogate of coronary
atherosclerosis: correlation with quantitative coronary angiography and
coronary intravascular ultrasound findings
Amato, M, et al. European Heart Journal (2007) 28, 2094-2101.
Distribution and Correlates of Sonographically Detected Carotid Artery Disease
in the Cardiovascular Health Study
O’Leary, DH, et al. Stroke 1992;23:1752-1760.
IMT to Predict Obstructive Disease and/or Coronary Calcium Score
Coronary Artery Calcium Versus Intima-Media Thickness as a Measure of
Cardiovascular Disease Among Asymptomatic Adults (from the Rancho Bernardo
Study)
Barrett-Connor, E, et al. Am J Cardiol 2007;99:227-231.
Carotid Artery Intima-Media Thickness could Predict the Presence of Coronary
Artery Lesions
Kotsis, T, et al. American Journal of Hypertension 2005;18:601-606.
Intima-media thickness of the common carotid artery is the significant predictor
of angiographically proven coronary artery disease
Holaj, R, et al. Can J Cardiol 2003;19(6):670-676.
Prediction of Coronary Heart Disease Using Risk Factor Categories
Wilson, W, et al. Circulation 1998;97:1837-1847.
IMT and Future Risk
Carotid Intima-Media Thickening Indicates a Higher Vascular Risk Across a Wide
Age Range
Prospective Date From the Carotid Atherosclerosis Progression Study (CAPS)
Lorenz, MW, et al. Stroke 2006;37:87-92 (4 years)
Comparison Between Measures of Atherosclerosis and Risk of Stroke
The Rotterdam Study
Hollander, M, et al. Stroke 2003;34:2367-2373. (6 years)
Ultrasonographically Assessed Carotid Morphology and the Risk of Coronary Heart
Disease
Salonen, JT, and Salonen, R.
Arteriosclerosis and Thrombosis 1991;11:1245-1249. (1 year)
Carotid-Artery Intima and Media Thickness as a Risk Factor for Myocardial
Infarction and Stroke in Older Adults
O’Leary, DH, et al. New England Journal of Medicine 1993;340:14-22. (6 years)
Association of Coronary Heart Disease Incidence with Carotid Artery Wall
thickness and Major Risk Factors: The Atherosclerosis in Communities (ARIC)
Study, 1987-1993
Chamblis, LE, et al. American Journal of Epidemiology 1997;146:483-94 (4-7
years)
Carotid Intima-Media Thickness as a Marker of Cardiovascular Risk in
Hypertensive Patients with Coronary Artery disease
Zielinski, T, et al. American Journal of Hypertension 2007;20:1058-1064. (5
years)
The role of Carotid Arterial Intima-Media Thickness in Predicting Clinical
Coronary Events
Hodis, HN, et al. Annals of Internal Medicine 1998;128:262-269.
C-Reactive Protein, Carotid Intima-Media Thickness, and Incidence of Ischemic
Stroke in the Elderly
Cao, J, et al. Circulation 2003;108:166-170.
Coronary Artery Calcium, Carotid Artery Wall thickness and Cardiovascular
Disease Outcomes in Adults 70 to 99 Years Old
Newman, A, et al. Am J Cardiol. 2008 January 15;101(2):186-192.
Effect of Carotid Atherosclerosis Screening on Risk Stratification During
Primary Cardiovascular Disease Prevention
Bard, R, et al. Am J Cardiol 2004;93:1030-1032.
Ultrasound B-Mode Imaging in Observational Studies of Atherosclerotic
Progression
Salonen, JT and Salonen, R.
Circulation 1993;87(suppl II):II-56-II-65) (2 years)
Endothelial Function and IMT
Interrelations Between Brachial Endothelial Function and Carotid Intima-Media
Thickness in Young Adults (the Cardiovascular Risk in Young Finns Study)
Juonala, M, et al. Circulation 2004;110:2918-2923.
Relationship between endothelial dysfunction, intima media thickness and
cardiovascular risk factors in asymptomatic subjects
Corrado. E, et al. International Angiology 2005;24:52-58.
Comparison of the Effects of Quinapril and Losartan on Carotid Artery Intima-Media
thickness in Patients with Mild-to-Moderate Arterial Hypertension
Uchiyama-tanake, Y, et al. Kidney and Blood Pressure Research 2005;28:111-116.
Plasma levels of asymmetric dimethylarginine (ADMA) are related to intima-media
thickness of the carotid artery - An epidemiological study
Furuki, K, et al. Atherosclerosis 191 (2007) 206-210.
Endocrine Function and IMT
Estrogen in the Prevention of Atherosclerosis
A Randomized, double-blind, Placebo-Controlled Trial
Hodis, HN, et al. Annals of Internal Medicine 2001; 135: 939-953.
Effect of Levothyroxine Replacement on Lipid Profile and Intima-Media thickness
in subclinical Hypothyroidism: A Double-blind, Placebo-controlled Study
Monzani, F, et al. Journal of Clinical Endocrinology & Metabolism 89 (5):
2099-2106.
The effects of Simvastatin and Levothyroxine on intima-media thickness of the
carotid artery in female normolipidemic patients with subclinical hypothyroisism:
a prospective, randomized-controlled study
Duman, D, et al. Journal of Cardiovascular Medicine 2007, 8:1007-1011.
Metformin of gliclazide, rather than glibenclamide, attenuate progression of
carotid intima-media thichkness in subjects with type 2 diabetes
Katakami, N, et al. Diabetologia (2004) 47:1906-1913.
Raloxifene slows down the progression of intima-media thickness in
post-menopausal women
Colaccurci, N, et al. Menopause Vol. 14, No. 5, pp. 879-884.
Effect of Rosiglitazone on Common Carotid Intima-Media Thickness Progression in
Coronary Artery Disease patients Without Diabetes Mellitus
Sidhu, J, et al. Arterioscler thromb Vasc Biol. 2004;24:930-934.
Effect of Peroxisome Proliferator-Activated Receptor
g
Agonist Treatment on subclinical Atherosclerosis in Patients With
Insulin-Requiring type 2 Diabetes
Hodis, H, et al. Diabetes Care 29:1545-1553, 2006.
Association Between Serum Testosterone Concentration and Carotid Atherosclerosis
in Men With Type 2 Diabetes
Fukui, M, et al. Diabetes Care 26:1869-1873, 2003.
Endogenous Sex Hormones and Progression of Carotid Atherosclerosis in Elderly
Men
Muller, M, et al. Circulation 2004;109:2074-2079.
Inflammation, Infection, and IMT
Association of Endotoxemia With Carotid Atherosclerosis and Cardiovascular
Disease
Prospective Results from the Bruneck Study
Wiederman, C, et al. J Am Coll Cardiol 1999;35:1975-1981.
Reduced Progression of Early Carotid Atherosclerosis After Antibiotic Treatment
and Chlamydia pneumonia Seropositivity
Sander, D, et al. Circulation 2002;106:2428-2433.
Increased Carotid Intima-Media thickness and Serum Inflammatory Markers in
Obstructive Sleep Apnea
Minoguchi, K, et al. Am J Respir Crit Care Med Vol 172. Pp 625-630, 2005.
Impact of Infectious Burden on Progression of Carotid Atheroslcerosis
Espinola-Klein, C, et al. Stroke 2002;33:2581-2586.
Early Carotid Atherosclerosis in subjects With Periodontal Diseases
Soder, P, et al. Stroke 2005;36:1195-1200.
Allergic Rhinitis, Asthma, and Atherosclerosis in the Bruneck and ARMY Studies
Knoflach, M, et al. Arch Intern Med 2005;165:2521-2526.
Genetic and Acquired Inflammatory Conditions Are synergistically Associated With
Early Carotid Atherosclerosis
Markus, H, et al. Stroke 2006;37:2253-2259.
Other Factors affecting IMT progression
Standing at work and progression of carotid atherosclerosis
Krause, N, et al. Scand. J. Work Environ Health 2000;26(3):227-326.
Antibodies to Oxidized LDL in Relation to Intima-Media thickness in Carotid and
Femoral Arteries in 58-Year-Old subjectively Clinically Healthy Men
Hulthe, J, et al. Arterioscler Thromb Vasc Biol. 2001;21:101-107.
Association between elevated plasma total homocysteine and increased common
carotid artery wall thickness
Voutilainem, S, et al. Ann Med 1998; 30: 300-306.
Serum 25-hydroxyvitamin D3 concentrations and carotid artery intima-media
thickness among type 2 diabetic patients
Targher, G, et al. Clinical Endocrinology (2006) 65, 593-597.
Mercury accumulation and accelerated progression of carotid atherosclerosis: a
population-based prospective 4-year follow-up study in men in eastern Finland
Salonen, JT, et al. Atherosclerosis 148 (2000) 265-273.
Sustained Anxiety and 4-Year Progression of Carotid Atherosclerosis
Paterniti, S, et al. Arterioscler Thromb Vasc Biol. 2001;21:136-141.
Carotid Artery Intial-Medial thickening and Plasma Homocystein in Asymptomatic
Adults
Malinow, R, et al. Circulation 1993;87:1107-1113.
Common Carotid Intima-Media Thickness Predicts Occurrence of Carotid
Atherosclerotic Plaques
Zureik, M, et al. Arterioscler Thromb Vasc Biol. 2000;20:1622-1629.
Tea consumption Is Inversely Associated With Carotid Plaques in Women
Debette, S, et al. Arteriosclerosis, Thrombosis, and Vascular Biology
2008;28(2):353-359.
A Prospective Study of the Effects of Irradiation on the Carotid Artery
Muzaffar, K, et al. Larygoscope 110;1811-1814, 2000.
Intima-Media Thickness of the Common Carotid Artery in Highway Toll collectors
Erdogmus, B, et al. Journal of Clinical Ultrasound Vol. 34, No. 9, Nov-Dec.
2006.
Resumption of Spontaneous Erections in Selected Patients Affected by Erectile
Dysfunction and Various Degrees of Carotid Wall Alteration: Role of Tadalafil
Caretta, N, et al. European Urology 48 (2005) 326-332.
Hyperhomocysteinemia but Not the C677T Mutation of Methylenetetrahydrofolate
Reductase Is an Independent risk Determinant of Carotid Wall Thickening
The Perth Carotid Ultrasound disease Assessment Study (CUDAS)
McQuillan, B, et al. Circulation 1999;99:2383-2388.
Role of Lipoprotein(a) and Apolipoprotein(a) Phenotype in Atherogenisis
Prospective Results From the Bruneck Study
Kronenburg, F, et al. Circulation 1999;100:1154-1160.
Biological Gradient Between Long-Term Arsenic Exposure and Carotid
Atherosclerosis
Wang, CH, et al. Circulation 2002;105:1804-1809.
Arsenic Exposure from Drinking-water and Carotid Artery Intima-medial Thickness
in Healthy Young Adults in Bangladesh
Chen, Y, et al. J Health Popul Nutr 2006 June;24(2):253-257.
Marked Elevation of Myocardial Trace Elements in Idiopathic Dilated
Cardiomyopathy Compared With Secondary Cardiac Dysfunction
Frustaci, A, et al. J Am Coll Cardiol 1999;33:1578-1583.
Intake of Mercury From Fish, Lipid Peroxidation, and the Risk of Myocardial
Infarction and Coronary, Cardiovascular, and Any Death in Eastern Finnish Men
Salonen, J, et al. Circulation 1995;91:645-655.
Blood Lead Below 0.48 umol/L (10 mcg/dl) and Mortality Among US Adults
Menke, A, et al. Circualiton 2006;114:1388-1394.
Additive Statistical Effects of Cadmium and Lead on Heart-Related disease in a
North Carolina Autopsy Series
Voors, A, et al. Archives of Environmental Health March/April 1982 Vol. 37 (No.
2):98-102.
Role of Cadmium and Magnesium in Pathogenesis of Idiopathic Dilated
Cardiomyopathy
Smetana, R, and Glogar, D. Am Jour Cardiol August 1, 1986 Vol. 58:364-366.
Optimistic Attitudes Protect Against Progression of Carotid Atherosclerosis in
Healthy Middle-Aged Women
Matthews, K, et al. Psychosomatic Medicine 66:640-644 (2004)
Socioeconomic Status and Progression of Carotid Atherosclerosis
Lynch, J, et al. Arteriosclerosis, Thrombosis, and Vascular Biology
1997;17:513-519.
Interactions of serum copper, selenium, and low density lipoprotein cholesterol
in atherogenesis
Salonen, J, et al. BMJ Volume 302 30 March 1991 pp. 756-760.
Association of Hypoadiponectinemia With Coronary Artery Disease in Men
Kumada, M, et al. Arterioscler Thromb Vasc Biol. 2003;23:85-89.
Increased Carotid Artery Intima-Media Thickness in subjects With Primary
Hypoalphalipoproteinemia
Baldassarre, D, et al. Arterioscler Thromb Vasc Biol. 2002;22:317-322.
Impact of subclinical carotid atherosclerosis on incident chronic kidney disease
in the elderly
Chonchol, M, et al. Nephrol dial Transplant (2008) 1-6.
Kidney function and Progression of Carotid Intima-Media Thickness in a Community
Study
Desbien, A, et al. Am J Kidney Dis 51:584-593.
Treatment to Blunt IMT Progression (Pharmacologic)
Arterial Biology for the Investigation of the Treatment Effects of Reducing
Cholesterol (ARBITER) 2
A Double-Blind, Placebo-Controlled Study of Extended-Release Niacin on
Atherosclerosis Progression in Secondary Prevention Patients Treated With
Statins
Taylor, AJ, et al. Circulation 2004;110:3512-3517.
The effect of 24 months of combination statin and extended-release niacin on
carotid intima-media thickness: ARBITER 3
Taylor, AJ, et al. Current Medical Research and Opinion Vol. 22, No. 11, 2006,
2243-2250.
The effects of extended-release niacin on carotid intimal media thickness,
endothelial function and inflammatory markers in patients with the metabolic
syndrome
Thoenes, M, et al. Int J Clin Pract, November 2007, 61, 11, 1942-1948.
Reduction in Carotid Arterial Wall Thickness Using Lovastatin and Dietary
Therapy
A Randomized, controlled Clinical Trial ***
Hodis, HH< et al. Annals of Internal Medicine 15 March 1996 Volume 124 Issue 6
Pages 548-556.
Beneficial Effects of Colestipol-Niacin Therapy on the Common Carotid Artery
Two and Four-Year Reduction if Intima-Media Thickness Measured by Ultrasound
Blankenhorn, DH, et al. Circulation 1993;88:20-28.
Effect of Controlled Release/Extended Release Metoprolol on Carotid Intima-Media
Thickness in Patients with Hypercholesterolemia - A 3-Year Randomized Study
Wiklund, O, et al. Stroke 2002;33:572-577.
Effect of Probucol on elederly Hypercholesterolemic Patients in the FAST Study
Sawayama, Y, et al. Fukuoka Acta Medica 97(1):15-24, 2006.
Treatment to Blunt IMT Progression (Nutritional)
Antioxidant Supplementation in Atherosclerosis Prevention (ASAP) study: a
randomized trial of the effect of vitamins E and C on 3-year progression of
carotid atherosclerosis
Saolonen, JT, et al. Journal of Internal Medicine 2000: 248: 377-386.
Six-Year Effect of Combined vitamin C and E Supplementation on Atherosclerotic
Progression
Salonen, R, et al. Circulation 2003;107:947-953.
Pomegranate juice consumption for 3 years by patients with carotid artery
stenosis reduces common carotid intima-media thickness, blood pressure, and LDL
oxidation
Aviram, M, et al. Clinical Nutrition (2004) 23, 423-433.
Glisodin, A Vegetal SOD with Gliadin, as Preventative Agent vs. Atherosclerosis,
as Confirmed with Carotid Ultrasound-B Imaging
Cloarec, M, et al. European Annals of Allergy and Clinical Immunology – volume
39- n°2–’07.
Eicosapententaenoic acid reduces the progression of carotid intima-media
thickness in patients with type 2 diabetes
Mita, T, et al. Atherosclerosis 191 (2007) 162-167.
Effect of n-3 fatty acids on carotid atherosclerosis and haemostasis in patients
with combined hyperlipoproteinemia: A double-blind pilot study in primary
prevention
Baldassarre, D, et al. Annals of Medicine 2006;38:367-375.
Effect of Supplementary Antioxidant vitamin Intake on Carotid Arterial Wall
Intima-Media Thickness in a Controlled Clinical Trial of Cholesterol Lowering
Azen, SP, et al. Circulation 1996;94:2369-2372.
Decrease of carotid intima-media thickness in patients at risk to cerebral
ischemia after supplementation with folic acid, Vitamins B6 and B12
Till, U, et al. Atherosclerosis 181 (2005) 131-135.
Vitamin C consumption is associated with less progression in carotid intima
media thickness in elderly men: A 3-year intervention study
Ellingsen, I, et al. Nutrition, Metabolism, and Cardiovascular Diseases (2008)
1-7.
Antioxidant Effects of Tocotrienols in Patients with Hyperlipidemia and Carotid
Stenosis
Tomeo, A, et al. Lipids 30:1179-1183 (1995).
Long-term calorie restriction is highly effective in reducing the risk for
atherosclerosis in humans
Fontana, L, et al. PNAS April 27, 2004 Vol. 101 No. 17 6659-6663.
Influence of lifestyle modification on atherosclerotic progression determined by
ultrasonographic change in the common carotid intima-media thickness
Markus, R, et al. Am J Clin Nutr 1997;65:1000-1004.