Following your initial evaluation, or to monitor for any change in your health status that might occur over time, Dr. Roberts may recommend that you undergo one or more of the below described diagnostic studies. The color code indicates studies that are carried out in our office, or by other practitioners upon referral from Dr. Roberts.
Electrocardiogram (EKG) - The standard 12-lead EKG gives us heart rate and a definitive description of heart rhythm. Abnormalities in cardiac chamber size, left ventricular wall thickness, and electrolyte status may be suggested, as can the presence of a prior heart attack, or active coronary insufficiency. False positive and false negative (you had a heart attack but we can't see it on the EKG) findings are not uncommon; thus we rarely make a diagnosis solely on the basis of an abnormal EKG. More likely, an abnormal EKG will lead to a more definitive test, such as a cardiac echo or some form of stress testing.
Cardiac Ultrasound (Echo) - A transducer placed on the chest wall emits sound waves that reflect (echo) off cardiac structures. The reflected waves return to the transducer, and are then computer processed to provide a two dimensional picture of the heart. A separate set of sound waves will bounce off the red cells rushing through the heart (doppler study), providing us with information regarding the volume and direction of blood flow. The full doppler echo provides definitive information regarding cardiac chamber size, pump function (ejection fraction and segmental wall motion abnormalities due to prior heart attack), and whether the heart fills easily or is stiff (diastolic function). Valve function abnormalities can be diagnosed and the degree of valve narrowing (stenosis) or leakage (regurgitation) can be quantified. The accuracy of cardiac echo can be compromised in overweight individuals and in those with advanced emphysema. Dr. Roberts was the first Cardiologist in NW Ohio to utilize doppler echo and color doppler flow mapping; the same with stress echo, intraoperative echo, TEE, intraoperative TEE, and dobutamine echo imaging.
Stress EKG - While the 12-lead EKG may reveal a
prior heart attack, an EKG obtained at rest cannot tell us whether you have
a coronary narrowing that might compromise blood flow to the heart
muscle during exercise. When you exercise to the point where the supply of oxygenated
blood cannot keep up with the demands of the exercising heart muscle, the
EKG changes in a characteristic fashion termed "ST depression". During
a stress EKG, or "stress test", a 12-lead EKG is obtained at rest, and then
every minute  while you walk on a motorized treadmill. Most
Cardiologists use the Bruce Protocol, in which the treadmill speed and the
incline against which you walk increase every three minutes. Exercise
induced ST depression suggests the presence of a flow-restrictive,
hemodynamically significant coronary artery narrowing. How far you can
walk, and how far you can walk before ST depression occurs, gives us an idea
as to the extent and severity of the coronary disease present. The stress EKG is not a perfect
study. It can miss (be falsely negative in) single vessel, especially
non-severe, single vessel coronary disease, or if you are unable to exercise
long enough to bring out a flow insufficiency (This is all about supply and
demand - with exercise the demand of the heart muscle for oxygenated blood
increases. If a coronary artery narrowing prevents this increase in
blood supply, then a supply:demand mismatch occurs, manifested on the EKG
as ST segment depression. If you do not walk far enough to bring out
increased demand, then we will not see the sign of decreased supply - we
will not bring out ST depression). False positive (ST depression occurs but
your arteries are normal) stress EKG studies are quite common.
Patients with left ventricular hypertrophy (wall thickening due to high
blood pressure), mitral valve prolapse, and those taking digitalis or whose
potassium levels are low frequently display falsely positive EKG findings.
50% of normal women will have a falsely positive stress EKG. In men
with chest pain highly suggestive of coronary disease, an abnormal stress
EKG confirms the diagnosis. In women, or in men with atypical pain or
conditions associated with false positive EKG findings, an abnormal stress
EKG typically leads to a confirmatory exam, such as a stress echo or stress
nuclear study.
while you walk on a motorized treadmill. Most
Cardiologists use the Bruce Protocol, in which the treadmill speed and the
incline against which you walk increase every three minutes. Exercise
induced ST depression suggests the presence of a flow-restrictive,
hemodynamically significant coronary artery narrowing. How far you can
walk, and how far you can walk before ST depression occurs, gives us an idea
as to the extent and severity of the coronary disease present. The stress EKG is not a perfect
study. It can miss (be falsely negative in) single vessel, especially
non-severe, single vessel coronary disease, or if you are unable to exercise
long enough to bring out a flow insufficiency (This is all about supply and
demand - with exercise the demand of the heart muscle for oxygenated blood
increases. If a coronary artery narrowing prevents this increase in
blood supply, then a supply:demand mismatch occurs, manifested on the EKG
as ST segment depression. If you do not walk far enough to bring out
increased demand, then we will not see the sign of decreased supply - we
will not bring out ST depression). False positive (ST depression occurs but
your arteries are normal) stress EKG studies are quite common.
Patients with left ventricular hypertrophy (wall thickening due to high
blood pressure), mitral valve prolapse, and those taking digitalis or whose
potassium levels are low frequently display falsely positive EKG findings.
50% of normal women will have a falsely positive stress EKG. In men
with chest pain highly suggestive of coronary disease, an abnormal stress
EKG confirms the diagnosis. In women, or in men with atypical pain or
conditions associated with false positive EKG findings, an abnormal stress
EKG typically leads to a confirmatory exam, such as a stress echo or stress
nuclear study.
Stress Echo - Echo imaging of the heart is carried out at rest and immediately following treadmill exercise. During exercise, the heart's energy needs increase, so it must produce more ATP; to do this it will need more oxygenated blood. If a coronary artery narrowing precludes this increase in oxygen supply, then ATP production will cease within the segment of heart muscle supplied by the narrowed artery. Function of that region will fall off, and the post-exercise echo images will show hypokinesis (reduced thickening and inward motion) of that segment. We can usually determine which artery is blocked, as wall motion will be increased over segments served by open vessels, and abnormal over the segment of heart muscle served by the diseased artery. The larger and more severe the wall motion abnormality, the more extensive and severe will be the coronary disease that caused it. The stress echo also provides information regarding valve function and how exercise or coronary insufficiency might adversely effect valve function.
Dobutamine Echo (Dobutamine) - Let's say we want to carry out a stress EKG or stress echo study, but you are unable to reach your "target heart rate", a level of exercise sufficient to bring out a supply:demand mismatch. Let's say that you have bad knees or lung disease or just can't walk far enough. In this situation we will carry out a "chemical stress test", either a dobutamine echo or a persantine cardiolite study. Dobutamine is an adrenalin-like drug that increased your heart rate and the vigor with which your heart contracts (we use dobutamine for this purpose in the treatment of decompensated congestive heart failure). We start with a low dose of dobutamine (10 micrograms/kg body weight/minute), and then increase the dose every three minutes as we monitor your EKG for ST depression and your echo for a diagnostic segmental contraction abnormality. If the study becomes abnormal, the dobutamine infusion is stopped, your body metabolizes the dobutamine rapidly, and your heart rate returns to baseline. If chest pain develops or if we wish to neutralize the dobutamine effect rapidly, we can administer a beta-blocker agent such as propranolol or metoprolol, which will rapidly counteract the dobutamine effect. Dobutamine echo imaging is often used to assess your cardiac risk with non-cardiac surgery, as the dobutamine chemical stress closely mimics the adrenalin chemical stress that will occur during the surgical procedure.
Transesophageal Echo (TEE) - If overweight stature or lung disease prevent us from obtaining good quality echo images across the chest wall, or if detailed images of the mitral valve or atria are required, then TEE will be utilized. Echo images are obtained from a miniaturized echo transducer mounted on the tip of a gastroscope (the same device that a gastroenterologist uses to examine the wall of your stomach for ulcers or inflammation). The TEE study is carried out in a hospital setting on an out-patient basis. An IV is placed and you receive Fentanyl (a short acting narcotic to relax the muscles of your throat) and Versed (a short acting valium-like agent). The back of your throat is sprayed with a local anesthetic. When you are good and relaxed and the back of your throat is numb, the echoscope is inserted into the back of your mouth and we ask you to swallow the scope into your stomach. This step is associated with slight gagging but once the scope reaches your stomach the gagging will stop. During the TEE procedure your heart rate, rhythm, blood pressure, and oxygen saturation will be monitored by a nurse, who along with an echo tech, assist Dr. Roberts as he carries out the study. TEE is especially useful in the analysis of mechanical prosthetic mitral valves. The plastic and metal of these devices blocks the transmission of sound waves into the heart, "hiding" regions of the heart from observation. During TEE the echo crystal is positioned within the esophagus, immediately behind the mitral valve, allowing excellent visualization. The standard cardiac echo typically allows good visualization of the cardiac ventricles, the pumping chambers, but the atria, the storage chambers, are deeper within the chest and are not as well seen. In the condition of atrial fibrillation, when we are concerned about the development of clots within the atria, standard echo imaging is not helpful and instead we will turn to TEE. TEE is also helpful in the diagnosis of congenital heart defects, such as an atrial septal defect, or a not completely closed atrial septum, termed "patent foramen ovale" which can be associated with paradoxical embolism (a stroke due to a blood clot within the veins of the calf that drains to the right heart and then crosses through the defect into the left heart and from there to the brain).
Stress Perfusion Study (Stress Cardiolite)
- The stress echo combines treadmill stress testing with echo imaging of the
heart. Likewise, the stress perfusion study combines treadmill testing
with nuclear imaging of the heart. An IV is placed in your arm and you
exercise on a treadmill in standard fashion. At peak exercise a
radiation emitting tracer (typically Cardiolite but other tracers are used)
is injected into your IV. The tracer attaches to the red cells within
your blood. The now radio-labeled red cells drain from your arm back
to the right heart, then across the lungs to your left heart, and from there
into the arterial circulation. Some of the tracer will then flow into
your coronary arteries, the three arteries that serve the heart muscle, and
the heart muscle will take up the tracer. The heart is then scanned by
a radiation detector; the images obtained will reflect tracer uptake by the
heart, which in turn reflect blood flow to the heart. If one artery is
blocked and two arteries are open, the segment of heart
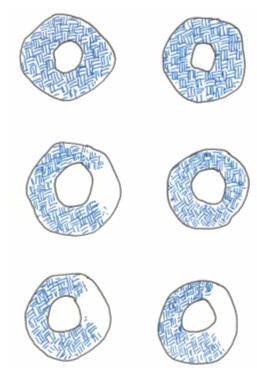 muscle
served by the blocked artery will receive relatively less radio-labeled
blood, will pick up relatively less Cardiolite, and will appear as a "cold
spot" on the images (left side of middle image on perfusion graphic). Four hours later
the heart is re-imaged. A segment of viable heart muscle that was
"cold" on the exercise images may now be seen to reperfuse or "fill in".
The artery did not open up, but over this four hour period enough
radio-labeled red cells were able to "wiggle through" the narrowing and
deposit their Cardiolite into the cells of the relatively underperfused
segment, allowing it to fill in on the four hour images (right side of middle
image).
Ischemia with reperfusion (a filling defect during exercise that resolves on
the resting images) indicates that a narrowed artery is compromising the
supply of oxygenated blood to a segment of viable, uninjured heart muscle. Now,
if the artery has closed and you have sustained a heart attack, if all of
the heart cells previously supplied by that artery have died, then your scan
will display a "fixed defect" on the post-exercise and four hour images
(bottom image). The artery is closed; the heart cells it once served
are dead. They will not pick up the tracer, and thus we see the fixed
defect. While there are exceptions to this rule, we would not
recommend a heart catheterization or attempt to revascularize a fixed defect
(the muscle is dead so there is nothing to save) while we will recommend
angiography or treatment when we see a reversible defect, because here we
have viable heart muscle at risk. Our goal with any therapy will be to
convert a reversible defect into a normal image (top graphic). This occurs with successful
EECP and was used as a measure of success in the early studies that
documented the benefit of this technique (see literature review in EECP
section). What we don't want to see is the conversion over time of a
reversible defect into a fixed defect; this means that the narrowed artery
has closed and that you have experienced a heat attack, that the jeopardized heart muscle has
now been lost. Recent advances in computer
imaging allow the reconstruction of the two dimensional images into a three
dimensional "perfusion picture" of the heart. Dual isotope study (a
different agent is injected on the resting study) allow us to shorten the
four hour delay into minutes, or to obtain the resting images first.
Still, the principles described above hold for all forms of stress perfusion
imaging. Stress perfusion imaging, like stress echo study, offers an
advantage over simple treadmill EKG study. False positive (the exam
looks abnormal but your arteries are really normal) studies are less
frequent. The nuclear technique is a little more sensitive (more
likely to pick up evidence of a blockage) such that we will have fewer false
negative (you have a blocked artery but we do not pick it up) studies.
Still, the nuclear imaging technique is not perfect. Soft tissue
(breast tissue in women and the abdominal organs in overweight men) will
absorb some of the radiation given off the cardiolite taken up by the heart muscle, leading to findings on the nuclear images
consistent with
a prior heart attack (this would be a false positive study). Slight
differences in the position of the breasts relative to the chest wall from
exercise to rest can lead to a (again false positive) diagnosis of coronary
ischemia. Individuals with left ventricular hypertrophy (muscle
thickening on the basis of hypertension or hypertrophic cardiomyopathy) or
left bundle branch block (a conduction disturbance seen on your resting EKG) may
also display perfusion defects in the presence of open arteries, as may
individuals with "Syndrome X", reduced blood flow to the heart muscle not on
the basis of fixed blockages, but instead on the basis of endothelial
dysfunction, impaired nitric oxide generation by the endothelial cells that
line our arteries. We keep these causes of false positive and false
negative nuclear studies in mind when deciding which technique, simple
stress EKG imaging, the stress echo, or the stress perfusion study, is best
suited to you as an individual. Dr. Roberts is well acquainted with
all three of these techniques. Dr. Roberts was the first cardiologist
in NW Ohio to carry out stress echo studies, and with a colleague
established the first cardiology-radiology nuclear stress study reading panel
(before that time all stress nuclear studies were read by radiologists,
without the input of a cardiologist). Dr. Roberts co-read half the
cardiac nuclear studies at his primary hospital for nearly a decade.
Dr. Roberts later dropped off the nuclear reading panel due to the
time commitments of his EECP and MME programs (and to be honest, Dr. Roberts has an
attention span of only 10 years). We do not have a nuclear camera in
the office. If we feel that a nuclear stress study is best for you,
then we will refer you to a practitioner who we trust for good studies and
good patient service. As a general rule, we prefer stress echo over
stress nuclear testing in overweight men and in well endowed women who
are set ups for a false positive nuclear scan, and when we are also
interested in looking at cardiac chamber size and valve function. We
favor nuclear imaging over stress echo study when lung disease or other
factors preclude us from obtaining good quality echo images of the heart.
muscle
served by the blocked artery will receive relatively less radio-labeled
blood, will pick up relatively less Cardiolite, and will appear as a "cold
spot" on the images (left side of middle image on perfusion graphic). Four hours later
the heart is re-imaged. A segment of viable heart muscle that was
"cold" on the exercise images may now be seen to reperfuse or "fill in".
The artery did not open up, but over this four hour period enough
radio-labeled red cells were able to "wiggle through" the narrowing and
deposit their Cardiolite into the cells of the relatively underperfused
segment, allowing it to fill in on the four hour images (right side of middle
image).
Ischemia with reperfusion (a filling defect during exercise that resolves on
the resting images) indicates that a narrowed artery is compromising the
supply of oxygenated blood to a segment of viable, uninjured heart muscle. Now,
if the artery has closed and you have sustained a heart attack, if all of
the heart cells previously supplied by that artery have died, then your scan
will display a "fixed defect" on the post-exercise and four hour images
(bottom image). The artery is closed; the heart cells it once served
are dead. They will not pick up the tracer, and thus we see the fixed
defect. While there are exceptions to this rule, we would not
recommend a heart catheterization or attempt to revascularize a fixed defect
(the muscle is dead so there is nothing to save) while we will recommend
angiography or treatment when we see a reversible defect, because here we
have viable heart muscle at risk. Our goal with any therapy will be to
convert a reversible defect into a normal image (top graphic). This occurs with successful
EECP and was used as a measure of success in the early studies that
documented the benefit of this technique (see literature review in EECP
section). What we don't want to see is the conversion over time of a
reversible defect into a fixed defect; this means that the narrowed artery
has closed and that you have experienced a heat attack, that the jeopardized heart muscle has
now been lost. Recent advances in computer
imaging allow the reconstruction of the two dimensional images into a three
dimensional "perfusion picture" of the heart. Dual isotope study (a
different agent is injected on the resting study) allow us to shorten the
four hour delay into minutes, or to obtain the resting images first.
Still, the principles described above hold for all forms of stress perfusion
imaging. Stress perfusion imaging, like stress echo study, offers an
advantage over simple treadmill EKG study. False positive (the exam
looks abnormal but your arteries are really normal) studies are less
frequent. The nuclear technique is a little more sensitive (more
likely to pick up evidence of a blockage) such that we will have fewer false
negative (you have a blocked artery but we do not pick it up) studies.
Still, the nuclear imaging technique is not perfect. Soft tissue
(breast tissue in women and the abdominal organs in overweight men) will
absorb some of the radiation given off the cardiolite taken up by the heart muscle, leading to findings on the nuclear images
consistent with
a prior heart attack (this would be a false positive study). Slight
differences in the position of the breasts relative to the chest wall from
exercise to rest can lead to a (again false positive) diagnosis of coronary
ischemia. Individuals with left ventricular hypertrophy (muscle
thickening on the basis of hypertension or hypertrophic cardiomyopathy) or
left bundle branch block (a conduction disturbance seen on your resting EKG) may
also display perfusion defects in the presence of open arteries, as may
individuals with "Syndrome X", reduced blood flow to the heart muscle not on
the basis of fixed blockages, but instead on the basis of endothelial
dysfunction, impaired nitric oxide generation by the endothelial cells that
line our arteries. We keep these causes of false positive and false
negative nuclear studies in mind when deciding which technique, simple
stress EKG imaging, the stress echo, or the stress perfusion study, is best
suited to you as an individual. Dr. Roberts is well acquainted with
all three of these techniques. Dr. Roberts was the first cardiologist
in NW Ohio to carry out stress echo studies, and with a colleague
established the first cardiology-radiology nuclear stress study reading panel
(before that time all stress nuclear studies were read by radiologists,
without the input of a cardiologist). Dr. Roberts co-read half the
cardiac nuclear studies at his primary hospital for nearly a decade.
Dr. Roberts later dropped off the nuclear reading panel due to the
time commitments of his EECP and MME programs (and to be honest, Dr. Roberts has an
attention span of only 10 years). We do not have a nuclear camera in
the office. If we feel that a nuclear stress study is best for you,
then we will refer you to a practitioner who we trust for good studies and
good patient service. As a general rule, we prefer stress echo over
stress nuclear testing in overweight men and in well endowed women who
are set ups for a false positive nuclear scan, and when we are also
interested in looking at cardiac chamber size and valve function. We
favor nuclear imaging over stress echo study when lung disease or other
factors preclude us from obtaining good quality echo images of the heart.
Persantine Cardiolite (Chemical Nuclear Stress Test) - This is another form of chemical stress testing. An IV is placed and Persantine (its generic name is Dipyridamole) is infused into an arm vein over four minutes. Persantine chemically dilates arteries, increasing their blood flow. Persantine will thus dilate the coronary arteries and will increase the flow of arterial blood to the heart muscle, that is, if the arteries are not blocked. Diseased arteries will not dilate in response to Persantine and blood flow to regions of heart muscle served by a diseased artery will not increase. Stated otherwise, in response to the IV administration of Persantine, blood flow to regions of heart muscle served by a diseased artery will be relatively decreased. During the third minute of the four minute Persantine infusion, a radiotracer such as Cardiolite will be injected into your IV. The Cardiolite will bind to circulating red cells, and just as in the treadmill stress perfusion study, the Cardiolite will be taken up by the heart muscle in relation to the blood flow that each region receives. During Persantine Cardiolite imaging, blood flow to a region of heart muscle served by a diseased artery will be relatively reduced compared to blood flow in adjacent regions served by open vessels. Cardiolite uptake will thus be less and we will see a segmental perfusion defect, just as we would on a treadmill exercise Cardiolite study carried out on the same patient. We utilize the Persantine study when we desire Cardiolite perfusion imaging in a patient who is unable to exercise on the treadmill. The conditions associated with false positive and false negative Persantine studies are the same as those that might compromise a treadmill stress Cardiolite exam - and there is one more. If all three of the coronary arteries serving your heart are narrowed to a similar degree, then blood flow to all three regions of the heart will be impaired in a uniform fashion. Cardiolite uptake, while absolutely decreased, will be uniform over the entire heart. When interpreting the perfusion images we are looking for a decrease in radiotracer uptake in one region relative to the others. In this situation, balanced three vessel coronary disease, tracer uptake will be uniform and your scan will be falsely normal. This could also occur on the images obtained when a patient with three vessel disease undergoes a treadmill stress perfusion study, but here we will also see marked ST segment depression and almost invariably a limited exercise capacity and significant effort induced symptoms of coronary insufficiency. These "tip offs" will not occur when a patient with three vessel disease undergoes a Persantine perfusion study. We see this problem about once a year, and we keep this possibility in mind. Most individuals experience mild chest tightness during the infusion of Persantine; this is an expected response and is not indicative of coronary disease. As the Persantine infusion is not producing an absolute reduction if coronary blood flow, we typically do not see ST segment depression. Should any problems occur during a Persantine study, we can instantly reverse the Persantine effect with the IV administration of a drug called Aminophylline (Aminophylline is also used to treat asthma). Caffeine will also inactivate Persantine, so if we have you scheduled for a Persantine study, it is important that you avoid all forms of caffeine (including chocolate) over the twenty four hours preceding the study.
Estrogen Metabolism - The pathways through which you activate and metabolize estrogen molecules play a key role in determining your risk of reproductive organ malignancy (breast, uterine, and prostate). We understand these pathways, how to assess them, and the interventions involved in optimizing your ability to metabolize estrogen. In this fashion we can add further safety to pellet bioidentical hormone replacement therapy.
Cardiac Catheterization
and Coronary Artery Angiography (Cath or Angio) - These invasive, hospital
based procedures allow precise definition of you cardiovascular physiology and coronary
artery anatomy - they are our diagnostic "gold standards". Cardiac catheterization refers to the process of
inserting a catheter (a narrow plastic tube - basically a long IV catheter)
into a peripheral vessel and advancing it under fluoroscopic (X-ray)
guidance into the region of the heart. The procedure is carried out in a hospital
room dedicated to this purpose (the "cath lab"). You arrive at the
hospital two hours before the procedure. An IV is placed within an arm
vein and you receive Versed (a short-acting Valium like agent) and Benadryl
(to minimize the risk of an allergic reaction to the X-ray contrast dye that
we use). We numb up the skin over the femoral artery and vein,
puncture these vessels with a needle, and then through the needle thread a
flexible guide wire into the vessels. The needle is withdrawn and over
the guide wire we pass the heart catheters. Through the catheters we
can record the blood pressures within your heart chambers and obtain
valuable information not available from non-invasive testing (are you fluid
overloaded or volume depleted, do you have pulmonary hypertension on the
basis 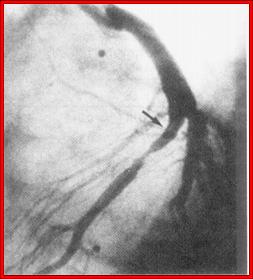 of
left heart failure or lung disease, how much blood is flowing through a
congenital defect in your heart, etc?). We can inject X-ray contrast
dye into the arteries that serve the heart while obtaining digital X-ray
images. This allows us to define the extent and severity of plaque
deposition within your coronary arteries. Afterwards the catheters are
withdrawn and manual (with our fingers) pressure is placed over the puncture
site to allow the artery to seal over. You then lie flat for 1 to 2
hours, and we typically send you home 3 hours later. With the
diagnostic information obtained from the catheterization/angiogram,
integrated in to what we know about you from your history, lab profile, and
non-invasive testing, we can make our best recommendation as to whether you
would benefit from a revascularization procedure, such as angioplasty/stent
placement, bypass surgery, laser revascularization, or EECP. The up
side of catheterization is that it the procedure gives us valuable
information. The down side is that it hurts a little (probably a
little worse than going to the dentist), and as catheterization/angiography
is an invasive procedure, it does expose you to some risk. The risk of
dieing from catheterization/angiography is 1 in 1000 and the risk of a
non-lethal complication is 1 in 100. Here we are talking about stroke
or heart attack due to clot formation or plaque dislodgement related to the
procedure itself, or damage to the femoral artery at the puncture site
(clotting or hematoma - a blood blister - formation). Your
catheterization related risk is related to your age and overall health.
Risk is greater when we are carrying out an urgent angiogram on an 80 year
old with unstable angina and pre-existent vascular and kidney disease.
Risk is much, much less when we are carrying out an elective procedure in a
younger patient in good health. The decision as to whether you should
or should not undergo catheterization is one that you will make with my
guidance. The key question is whether the value of the information
gained from the procedure will be worth the risk associated with the
procedure. Most often the decision is straight forward and easy to
make. Other times we will scratch our heads and consider other
options. In general, if a non-invasive approach will give us the
information that we need, then we will not carry out an angiogram.
However, if we feel that you might benefit from an invasive
revascularization procedure, than an invasive diagnostic procedure, the
angiogram, is mandatory. A surgeon cannot carry out bypass surgery
without an angiogram to guide him - otherwise how would he know where to
place the grafts? You can't be stented based on a stress test alone.
Sometimes, based on my non-invasive assessment, I just can't be sure whether
or not you have a blocked artery. You may not be interested in
invasive revascularization, but before we spend a great deal of your
out-of-pocket money on non-interventional, complementary approaches,
shouldn't we also definitively determine whether you do or do not actually
have a blockage? Many of you are fearful of the angiogram, not just
over the risk associated with the procedure, but over what will come next.
You are fearful that once we get you into the hospital setting, that we will
not let you go without an invasive revascularization procedure. This
fear is justified. If a narrowing is found, pressure was placed on
me to recommend a stent or bypass surgery. Pressure will be placed on
you to undergo a procedure. The people who work in our hospitals are
all good people, but the only approach to cardiovascular disease that they
know about is invasive/interventional. This is what they do, day in
and day out. This is what they are good at. They work hard and
they help people so this is their approach to cardiovascular care.
They do not know anything about chelation therapy, EECP, MME, IV
phosphatidylcholine therapy, mitochondrial support or homeopathy. They
don't know the first thing about these modalities and are convinced that
these complementary techniques cannot help you. They feel that the
only way to get better is via an invasive approach. You may hear
something like - "If you leave the hospital without bypass surgery you will
have a heart attack and die". I know what they say because this is
what I said to patients over the first 10 years of my career. I said
this because I didn't know that other (and often better) options were
available - but now I do. I will recommend an invasive procedure if my
need to know outweighs the risks (to you as an individual) associated with
the procedure. I have carried out thousands of invasive cardiac
studies, but as my focus shifted away from crisis management and towards
dealing with the causes of vascular disease, the number of my patients
requiring angiography steadily decreased. I also became uncomfortable with
the way I was being treated by doctors, nurses, and hospital administrative
staff (the wonderful exception here are the nurses at the Toledo Hospital
Catheterization Lab - all skilled, professional, and pleasant people to work
with) so I quit carrying out angiograms and left the hospital forever.
If you are my patient and I feel you need an invasive study, I will organize
your records and communicate in writing with an invasive cardiologist who I
trust. They will carry out your angiographic study, then proceed with stent
placement or referral for bypass surgery, if these steps are appropriate. I
will receive a report and then get re-involved in your care following your
recovery.
of
left heart failure or lung disease, how much blood is flowing through a
congenital defect in your heart, etc?). We can inject X-ray contrast
dye into the arteries that serve the heart while obtaining digital X-ray
images. This allows us to define the extent and severity of plaque
deposition within your coronary arteries. Afterwards the catheters are
withdrawn and manual (with our fingers) pressure is placed over the puncture
site to allow the artery to seal over. You then lie flat for 1 to 2
hours, and we typically send you home 3 hours later. With the
diagnostic information obtained from the catheterization/angiogram,
integrated in to what we know about you from your history, lab profile, and
non-invasive testing, we can make our best recommendation as to whether you
would benefit from a revascularization procedure, such as angioplasty/stent
placement, bypass surgery, laser revascularization, or EECP. The up
side of catheterization is that it the procedure gives us valuable
information. The down side is that it hurts a little (probably a
little worse than going to the dentist), and as catheterization/angiography
is an invasive procedure, it does expose you to some risk. The risk of
dieing from catheterization/angiography is 1 in 1000 and the risk of a
non-lethal complication is 1 in 100. Here we are talking about stroke
or heart attack due to clot formation or plaque dislodgement related to the
procedure itself, or damage to the femoral artery at the puncture site
(clotting or hematoma - a blood blister - formation). Your
catheterization related risk is related to your age and overall health.
Risk is greater when we are carrying out an urgent angiogram on an 80 year
old with unstable angina and pre-existent vascular and kidney disease.
Risk is much, much less when we are carrying out an elective procedure in a
younger patient in good health. The decision as to whether you should
or should not undergo catheterization is one that you will make with my
guidance. The key question is whether the value of the information
gained from the procedure will be worth the risk associated with the
procedure. Most often the decision is straight forward and easy to
make. Other times we will scratch our heads and consider other
options. In general, if a non-invasive approach will give us the
information that we need, then we will not carry out an angiogram.
However, if we feel that you might benefit from an invasive
revascularization procedure, than an invasive diagnostic procedure, the
angiogram, is mandatory. A surgeon cannot carry out bypass surgery
without an angiogram to guide him - otherwise how would he know where to
place the grafts? You can't be stented based on a stress test alone.
Sometimes, based on my non-invasive assessment, I just can't be sure whether
or not you have a blocked artery. You may not be interested in
invasive revascularization, but before we spend a great deal of your
out-of-pocket money on non-interventional, complementary approaches,
shouldn't we also definitively determine whether you do or do not actually
have a blockage? Many of you are fearful of the angiogram, not just
over the risk associated with the procedure, but over what will come next.
You are fearful that once we get you into the hospital setting, that we will
not let you go without an invasive revascularization procedure. This
fear is justified. If a narrowing is found, pressure was placed on
me to recommend a stent or bypass surgery. Pressure will be placed on
you to undergo a procedure. The people who work in our hospitals are
all good people, but the only approach to cardiovascular disease that they
know about is invasive/interventional. This is what they do, day in
and day out. This is what they are good at. They work hard and
they help people so this is their approach to cardiovascular care.
They do not know anything about chelation therapy, EECP, MME, IV
phosphatidylcholine therapy, mitochondrial support or homeopathy. They
don't know the first thing about these modalities and are convinced that
these complementary techniques cannot help you. They feel that the
only way to get better is via an invasive approach. You may hear
something like - "If you leave the hospital without bypass surgery you will
have a heart attack and die". I know what they say because this is
what I said to patients over the first 10 years of my career. I said
this because I didn't know that other (and often better) options were
available - but now I do. I will recommend an invasive procedure if my
need to know outweighs the risks (to you as an individual) associated with
the procedure. I have carried out thousands of invasive cardiac
studies, but as my focus shifted away from crisis management and towards
dealing with the causes of vascular disease, the number of my patients
requiring angiography steadily decreased. I also became uncomfortable with
the way I was being treated by doctors, nurses, and hospital administrative
staff (the wonderful exception here are the nurses at the Toledo Hospital
Catheterization Lab - all skilled, professional, and pleasant people to work
with) so I quit carrying out angiograms and left the hospital forever.
If you are my patient and I feel you need an invasive study, I will organize
your records and communicate in writing with an invasive cardiologist who I
trust. They will carry out your angiographic study, then proceed with stent
placement or referral for bypass surgery, if these steps are appropriate. I
will receive a report and then get re-involved in your care following your
recovery.
Intravascular Ultrasound (IVUS) - The coronary angiogram gives us a silhouette of the artery. We define percent stenosis, the severity of the blockage, as our estimate of the degree of narrowing related to an adjacent region of the artery that is normal. This is a subjective assessment. I tend to "under-read" in comparison to the interventional cardiologists and cardiac surgeons who I work with. There is an old adage that in cardiology there are "under readers" and "over readers" and no "perfect readers". This is true. Our perception on your angiogram will be based on how we were trained to read angiograms. We often disagree a little, but what is important is that we are internally consistent (we interpret your angiogram films the same way, every time). Often we will pull up your old films and compare your current study with a previous exam (an apples to apples comparison). There are times, however, when we just can't be sure as to the severity of a narrowing. Perhaps the narrowing is on a bend or the artery is overshadowed by another vessel. Sometimes the entire artery is diseased, such that we do not have a "normal vessel" reference point against which to compare the narrowing under question. In these situations, when we have an important decision to make (should you or should you not undergo bypass surgery?), I may recommend that you undergo an IVUS procedure. Here the heart catheter has a tiny echo crystal at its tip. A small region of the vessel (the region of vessel at the tip of the catheter) can be precisely studied by ultrasound. A precise percent narrowing of the narrowing in question can be determined. The IVUS catheter is relatively large, and as such can only be used to quantitative proximal (at the beginning of a vessel) narrowings. It is typically used when we cannot determine from the angiogram alone whether you have a significant narrowing in the Left Main or Left Anterior Descending coronary arteries.
Electrophysiology Study (EPS) - EPS, an invasive diagnostic procedure, guides decision making in the management of complex cardiac arrhythmia. An electrode tipped catheter is advanced from the femoral vein in the groin into the right heart. Electrical recordings are made of the SA node (sinus node - the atrial pacemaker), the AV Node (the electrical junction between the atria and the ventricles), and the intra-atrial and intra-ventricular conduction pathways. Bypass tracts, areas of supra-normal conduction that underlie many supraventricular (originating within the atria or AV node) arrhythmias, can be detected. Provocative testing determines whether on not the electrical conduction system can propagate an abnormal signal over and over. PVCs (premature ventricular complexes - extra beats originating from the ventricles) are a nuisance, and only a nuisance, unless they can be strung together at a rapid rate over a prolonged period of time (ventricular tachycardia - a life threatening situation where the heart beats inefficiently at rates of up to 250 beats per minute). In provocative testing, short bursts of electrical impulses are fired from the right heart electrode catheter. If these cannot generate an episode of ventricular tachycardia, then your heart, on its own, cannot - in this situation you are not at risk for a potentially lethal arrhythmia. On the other hand, if ventricular tachycardia can be easily "induced", then your PVCs represent a threat, and require treatment, either with a drug or an implanted defibrillator. 90% of people with PVCs are not at risk for VT; they have otherwise normal hearts and their PVCs are not a threat. In patients with pre-existent advanced heart disease (prior heart attack or dilated cardiomyopathy), PVCs represent a potential threat and here EPS testing makes sense. If we see short runs of VT on your Holter study and we know that your heart pumping function is seriously impaired, then EPS testing is not even necessary - in this scenario placement of a permanent defibrillator makes sense. EPS is used when we have a rhythm-related question that needs to be answered. EPS may be followed by a catheter - based intervention, most frequently AV Node ablation to resolve AV nodal "re-entrant" arrhythmias. Here, the catheter tip is placed against the region of abnormal conduction, and "radio-frequency" ablation is carried out. Basically the tip of the catheter is heated up to destroy a pin-pint region of the heart's conduction system. Fib-ablation, to resolve atrial fibrillation, is available in regional centers, and in some individuals catheter based interventions can even resolve ventricular tachycardia.
24 Hour EKG Holter Monitor (Holter) - The standard 12-lead EKG gives us your cardiac rhythm at the moment the EKG was recorded, but it doesn't tell us what your rhythm was five minutes earlier, and it can't tell us what your rhythm is at home when you might be experiencing symptoms. The 24 hour Holter monitor is basically a 24 hour EKG. EKG leads are placed and fed into a tape recorder. You war the apparatus (which is not uncomfortable) over the next 24 hours while engaging in your usual activities. We provide you with a diary to record your symptoms as you experience them. The tape will be scanned and Dr. Roberts can then correlate your recorded symptoms with what your cardiac rate and rhythm were at the time that they occurred. The Holter study can also be used to monitor drug/nutritional therapy prescribed to treat a rhythm disturbance. The 12 led EKG can tell us whether a therapy has normalized your rhythm at one point in time, while the Holter study can tell us if we have controlled the arrhythmia all the time (at least over the 24 hours of the monitoring period).
Carotid Ultrasound - Similar to doppler echo study of the heart - a transducer placed over the neck bounces sound waves off the walls of the carotid artery, with a second set directed at the red cells flowing up the carotid artery into the brain. Plaque deposition within the walls of the carotid artery, narrowing the vessel, can be directly visualized. The speed with which the red cells course through the artery can also be used to estimate the degree of narrowing. Keeping in mind the analogy of your finger over the end of a garden hose, the narrower the vessel, the faster the red cells must flow. If moderate, non-threatening disease is identified, we will likely repeat your scan on a yearly basis. A progressive rise in carotid artery flow velocity means that the artery is narrowing, that you are laying down more plaque. A decrease in carotid flow velocity means that your artery is opening up. The carotid ultrasound gives us anatomy and flow rate, but it doesn't give us endothelial function, and it doesn't differentiate vulnerable from stable plaque. You can have a stroke when a vulnerable 40% plaque ruptures. Tiny ulcers within a non-obstructive plaque can release small platelet clots that lead to TIAs (transient ischemic attacks). You can close off a carotid artery slowly, forming collaterals from the opposite side, and never experience a stroke (just as collateral vessels within the coronary vasculature can allow you to close off an artery without functional consequence). Thus in decision making we consider the carotid ultrasound findings along with your symptoms and other test results. The carotid ultrasound is painless and risk free. Surgeons will operate based on a good quality scan demonstrating a high-grade narrowing; a confirmatory carotid angiogram is usually not needed.
Carotid Artery
Intima-Media Thickness (IMT) - In the standard carotid ultrasound
study, sound waves are directed at the entire carotid artery and at the red
cells flowing through it. In carotid artery IMT testing, the sounds
waves are focused on a single region, the back wall of this vessel, allowing
a crystal clearer picture of this region. The thickness of the intima
(the inner lining of the vessel, which included the endothelial cells) and
the media (the middle muscular layer of the artery), can be precisely
quantified. The IMT of your carotid artery is a good measure of plaque
build up in your entire circulation. It correlates with plaque
disposition within your coronary arteries, and your risk for an adverse
cardiovascular event.
 Of greater importance,
the rate of change in your carotid artery IMT measurement reflects that rate
at which all the arteries in your body are filling up with plaque.
Serial IMT measurement is a great way for us to monitor your status and to
asses the effect of our treatments. Think of the IMT as the "staging
ground" for obstructive plaque. The attached graph depicts change
in IMT over time in individuals taking Vitamins C and E vs. placebo.
As you can see, disease progression was more rapid in the placebo group.
Carotid IMT looks at soft plaque, the metabolically active plaque, while
coronary artery calcium scoring looks only at "hard plaque", less
metabolically active arterial calcification. The Carotid artery IMT
study is risk-free, informative, relatively low in cost, and it doesn't
require a hospital based procedure, so as you would predict, its cost is
typically not covered by insurance (while they never hesitate to cover the
cost of invasive, hospital based diagnostic procedures). Thus Carotid
IMT testing represents an out-of-pocket expense to you, but it is quite
informative and worth the $200. For more information click
Carotid Artery
Intima-Media Thickness (IMT).
Of greater importance,
the rate of change in your carotid artery IMT measurement reflects that rate
at which all the arteries in your body are filling up with plaque.
Serial IMT measurement is a great way for us to monitor your status and to
asses the effect of our treatments. Think of the IMT as the "staging
ground" for obstructive plaque. The attached graph depicts change
in IMT over time in individuals taking Vitamins C and E vs. placebo.
As you can see, disease progression was more rapid in the placebo group.
Carotid IMT looks at soft plaque, the metabolically active plaque, while
coronary artery calcium scoring looks only at "hard plaque", less
metabolically active arterial calcification. The Carotid artery IMT
study is risk-free, informative, relatively low in cost, and it doesn't
require a hospital based procedure, so as you would predict, its cost is
typically not covered by insurance (while they never hesitate to cover the
cost of invasive, hospital based diagnostic procedures). Thus Carotid
IMT testing represents an out-of-pocket expense to you, but it is quite
informative and worth the $200. For more information click
Carotid Artery
Intima-Media Thickness (IMT).
Electromyelogram (EMG) - The EMG is a non-invasive measure of peripheral nerve function. Tiny electrodes are placed over points along the course of a nerve, a current is applied, and the timing and quality of the conducted impulse are measured. EMG testing allows us to localize the point of nerve damage or impingement (if your hand is weak and clumsy, is the problem in the carpal tunnel, in the elbow region, or within the cervical spine?). If you present with upper or lower extremity symptoms, the EMG evaluation will help us determine whether they are vascular or neurological in etiology (cause).
Evaluation of Toxicity - Approaches to Detoxification (All discussed in more detail below)
Heavy Metal Provocative Challenge Study (Triple Challenge) - The Triple Challenge is our best measure of your total body toxic metal burden (also see discussion in Treatments Available - Chelation Therapy section). Over the three days preceding the exam, and on the day of the exam, you take Med Five (enteric-coated EDTA and phosphatidylcholine) twice a day, to saturate your GI tract with metal binders. The test itself involves the IV administration of 1000 mg of Calcium-EDTA and 125 mg of DMPS (sometimes we use 250 mg or oral DMPS instead) along with the oral administration of 500 mg of DMSA and 1000 mg of Vitamin C. Urine is collected over the next six hours, and a sample is then sent to Doctor's Data in Chicago for analysis (see representative challenge results). Their turn around time is 1-2 weeks. The triple challenge is typically well tolerated, but you may feel a little punk that day, as toxins are mobilized from deep tissue stores. We are giving you IV pharmacologic agents, so there is the potential for an allergic reaction, but we have carried out hundreds of these studies and have never observed this. To be on the safe side, you will remain in the office for fifteen minutes following administration of the IV agents, under observation; you leave only if you and we feel that you are OK. We encourage you to drink extra water on the day of your Triple Challenge. Diluting the urine with extra fluids is not a problem, as Doctor's Data reports the level of each metal in relation to micrograms of creatinine present (this corrects for any dilution effect). Factors influencing just which metals are brought out and at what level are discussed in the Chelation Therapy section. The Triple Challenge results will be integrated into your overall evaluation and used to determine which approach to heavy metal detoxification (if any) is appropriate for you. We can also carry out challenges using only EDTA, typically at 3000 mg instead of at 1000 mg Triple Challenge dose; here we would be looking at Lead and Cadmium and pretty much ignoring Mercury. A DMPS (only) challenge would involve the administration of 250 mg of IV DMPS, and would bring out relatively more Mercury and relatively less Lead and Cadmium. We can also carry out "Double Challenges", combining oral DMSA with IV EDTA or IV DMPS. Our standard approach, however, is to use the Triple Challenge as our measuring stick. The cost of a Triple Challenge is $185 including the lab fee. You do need to sign an informed consent form. Insurance will not cover the cost of the Triple Challenge; this will be an out-of-pocket expense to you. Insurance typically will cover the cost of blood tests for heavy metals, but these bear little relationship to your body burden of a given toxic metal and are not of value in decision making (again see discussion in the Chelation Therapy section).
Peripheral Vascular Study (PVR) - PVR testing diagnoses the presence of, and then quantifies the severity of, vascular insufficiency within the lower extremities. BP values are obtained over the arm, the thigh, and the ankle. In the absence of lower extremity vascular disease, the ratio of blood pressure between the arm and ankle (the ankle brachial index or ABI) will be one or close to one. In the presence of lower extremity vascular insufficiency, the ratio will be below one; the lower the ratio, the more severe the disease. Changes in large artery lower extremity blood flow in response to treatment will be mirrored by changes in one's PVR values. When vascular disease is obvious, a resting PVR study suffices to document the severity of vascular insufficiency. Rest and post-exercise PVR study may bring out evidence of early disease.
Ultrafast CT Scan for Calcium Scoring - This is a rapid CT scan of the chest that can quantitative the amount of calcium in your coronary arteries. Normal arteries contain no calcium (Dr. Roberts' calcium score was zero). An artery diseased with atherosclerotic plaque will contain calcium within its wall - the larger the volume of plaque, the greater will be the degree of calcification, the higher will be the calcium score. A calcium score of 100 is often used to differentiate "high risk" from a "low risk" scan, but there are many exceptions to this rule. Atherosclerosis is common in Americans, and thus we expect to see higher calcium scores in the elderly as opposed to in younger individuals - and we do. Coronary artery calcification worsens over time, on average by 45% per year. Thus a calcium score of 100 in an 80 year old man is not a surprise and in general does not suggest a severe coronary narrowing, while the same score in a 30 year old would cause great alarm. Patients whose calcium scores progress rapidly are at increased risk for an adverse clinical event (this makes sense - their plaque volume is progressing rapidly), while individuals whose scores are stable or only slowly increasing will not have events. So far the only therapies that have been shown to slow down the rate of coronary calcification are antioxidants and statin cholesterol lowering (and anti-inflammatory) agents. NanobacEDTA is the only therapy that has been shown to potentially reverse the calcium score. In thinking about the calcium score, keep in mind that the score reflects the volume of calcified atherosclerotic plaque, not the volume of "soft plaque", and not the architecture of the arteries. A high score does not mean that an artery contains a high grade narrowing. The calcium score in no way reflects endothelial function, which determines your short and long-term outcome, and the calcium score cannot differentiate vulnerable from stable plaque. Dr. Roberts has found occluded vessels in patients with calcium scores of zero - the articles say that this is not supposed to happen but we see this. Conversely, we have studied older patients with scores well above 500 who have only mild plaqueing on their angiograms. We thus do not make decisions solely on the calcium score.
64 Slice CT Scan - This CT scan provides a
fairly good image of the flow area of the coronary arteries, and is designed
to serve as a "non-invasive angiogram". If the scan is normal you are
in good shape, and if it shows an occluded artery then you probably have an
occluded artery or at least a high-grade narrowing. In between there
is somewhat of a grey zone. The 64 slice CT also provides a calcium
score. If the degree of calcification is extensive, say above 1000,
then the accuracy of the arterial images falls off markedly. Insurers
will not cover this study, and it costs about $500. If I think, based
upon an abnormal stress imaging study, that you have an important narrowing
and recommend a coronary angiogram and you decide instead to undergo a 64
slice CT study, well, if the scan is normal or shows only minimal disease,
then you are not at risk and I will back down on my recommendation that you
undergo an angiogram. If instead, a moderate narrowing is described on
the scan, then an angiogram will still be needed, as here the CT scan does
not provide precise enough information for decision making (especially is
extensive calcification is present). We certainly cannot make a
decision to proceed with stent placement or bypass surgery based upon the 64
slice or calcium scoring CT scan alone.
Methyl Cycle NutriGenomic Testing and Therapy - This is the Medicine of the future and we are pleased to add Nutrigenomic Testing and Therapy to our practice in 2008. At this time we have the capability of measuring the commonly encountered genetic defects within the Methyl Cycle. Think of the Methyl Cycle as the backbone of our physiology. We need Methyl Cycle intermediates to ward off viral and bacterial infection, to properly decode our DNA, and to protect ourselves from environmental toxins. Methyl Cycle abnormalities explain why one person becomes toxic from the environment while others in the same environment continue to enjoy good health. Autistic kids harbor Methyl Cycle defects - this is why they can't handle the Mercury (and other toxins) that they were exposed to, while other kids can. It's not just the toxicity or the degree of toxicity; rather it's the presence of any toxicity in a kid who genetically cannot handle it. Kids with neurodevelopmental abnormalities, adults with premature "diseases of aging", cardiac patients with elevated homocysteine levels not responding to standard B vitamin supplementation, and individuals with paradoxical responses to treatments are all good candidates for Methyl cycle Genomic Testing, as are smart people who want to know their genetic weak links before they become ill due to them.
James C. Roberts MD FACC FAARFM
2/13/18