Return to Treatments Available
Page
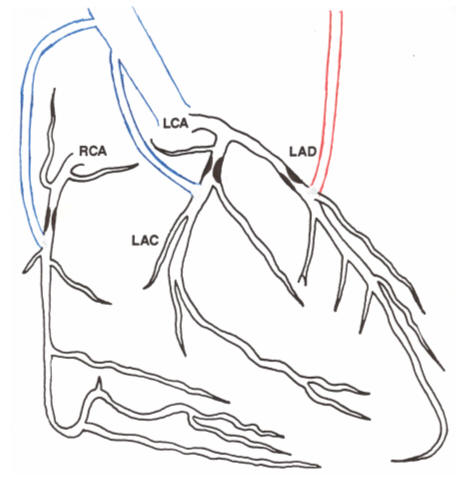
Coronary Artery Bypass Surgery (CABG) - CABG provides direct, anatomic
revascularization. CABG is standard cardiology's most effective, "sure
thing" approach to coronary insufficiency. Here the problem is looked at
as a supply:demand mismatch, a mismatch between the supply of oxygenated blood
to the heart muscle and the demand of the heart muscle for oxygenated blood.
CABG correct the mismatch. Superficial veins are removed from the surface
of your legs, cleaned of surrounding tissues, and then a short segment of vein,
reversed in orientation (veins allow only one way flow), is used as a bypass
conduit. One end is sewn into the aorta, the great vessel that conveys
oxygenated blood away from the heart. The other
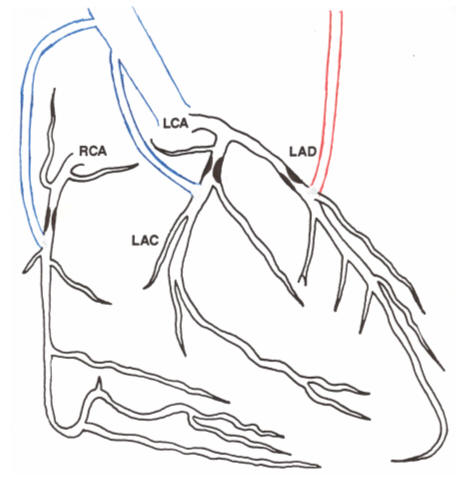 end
is sewn into a diseased coronary artery, beyond its point of blockage,
"bypassing" the blockage. Oxygenated blood is thus resupplied to a
previously oxygen starved region of heart muscle. Energy production will
normalize and your symptoms will resolve. Whenever possible, surgeons will
utilize arterial grafts during CABG. The left internal mammary artery
originates from the left subclavian artery (which goes on to supply the left
upper extremity). The left internal mammary artery (LIMA) normally
provides oxygenated blood to the left upper chest wall. When used as a
bypass conduit, the proximal end of the LIMA is left attached to the left
subclavian artery. The small side branches given off the LIMA to supply
the chest wall musculature are tied off. The distal end of the LIMA is
mobilized away from the chest wall and is then sewn into a coronary artery,
usually the left anterior descending (LAD), "bypassing" the blockage.
Blood flow will take the path of least resistance, so following bypass surgery
the narrowing in the diseased but now bypassed native artery will often close,
but that is not an issue, as the wide open graft will supply all the oxygenated
blood that is required. The superficial leg veins were designed to
transport deoxygenated, or "used" blood from the cells of the leg back to the
heart, for later re-oxygenation as the used blood flows through the lungs.
The superficial leg veins are actually responsible for only 15% of lower
extremity return blood flow. The deep veins are responsible for the
other 85%. They are left intact, so ankle swelling is typically not a
problem following CABG in young people. Older patients may need to wear
support stockings following bypass surgery, but this is not a huge price to pay.
The real problem with vein grafts is that we are asking a vein to do an artery's
job (more on this later). The chest wall also receives arterial blood from
vessels that originate in the abdomen. Following bypass surgery that
utilizes the LIMA, patients often note a vague discomfort over the chest wall.
This sensation is sometimes difficult to differentiate from your prior angina,
because it is mild "angina" of the chest wall, as it's blood supply has been
reduced. This is not a threat and the discomfort is only minor, and is not
a cause of worry.
end
is sewn into a diseased coronary artery, beyond its point of blockage,
"bypassing" the blockage. Oxygenated blood is thus resupplied to a
previously oxygen starved region of heart muscle. Energy production will
normalize and your symptoms will resolve. Whenever possible, surgeons will
utilize arterial grafts during CABG. The left internal mammary artery
originates from the left subclavian artery (which goes on to supply the left
upper extremity). The left internal mammary artery (LIMA) normally
provides oxygenated blood to the left upper chest wall. When used as a
bypass conduit, the proximal end of the LIMA is left attached to the left
subclavian artery. The small side branches given off the LIMA to supply
the chest wall musculature are tied off. The distal end of the LIMA is
mobilized away from the chest wall and is then sewn into a coronary artery,
usually the left anterior descending (LAD), "bypassing" the blockage.
Blood flow will take the path of least resistance, so following bypass surgery
the narrowing in the diseased but now bypassed native artery will often close,
but that is not an issue, as the wide open graft will supply all the oxygenated
blood that is required. The superficial leg veins were designed to
transport deoxygenated, or "used" blood from the cells of the leg back to the
heart, for later re-oxygenation as the used blood flows through the lungs.
The superficial leg veins are actually responsible for only 15% of lower
extremity return blood flow. The deep veins are responsible for the
other 85%. They are left intact, so ankle swelling is typically not a
problem following CABG in young people. Older patients may need to wear
support stockings following bypass surgery, but this is not a huge price to pay.
The real problem with vein grafts is that we are asking a vein to do an artery's
job (more on this later). The chest wall also receives arterial blood from
vessels that originate in the abdomen. Following bypass surgery that
utilizes the LIMA, patients often note a vague discomfort over the chest wall.
This sensation is sometimes difficult to differentiate from your prior angina,
because it is mild "angina" of the chest wall, as it's blood supply has been
reduced. This is not a threat and the discomfort is only minor, and is not
a cause of worry.
The short term down side of CABG is the surgical risk, which varies with your
age and overall health. Younger patients in otherwise good health cruise
right through CABG and may be discharged home on their 5th post-operative day.
Elderly patients in otherwise poor health are at risk for surgical complications
involving their brain, kidneys, and other internal organs. Applying the
principles of nutritional cardiology will unequivocally reduce your surgical
risk and hasten your discharge from the hospital, but such therapies are
forbidden in nearly all US hospitals. I am totally serious here - numerous
studies published in peer reviewed cardiology journals tell us that agents such
as magnesium, Co-enzyme Q10, vitamin C, and ribose lower mortality, reduce
complication rates, and get you out of the hospital faster following CABG.
However, their use is not permitted in our hospitals. If I wrote an order
for Co-enzyme Q10 or vitamin C in a patient scheduled for CABG, the nurse would
not honor it, the patients would be told that I wrote an order that was against
hospital policy, and I would get a stupid phone call from the pharmacy
technician telling me that these agents are "unproven homeopathic" substances.
Dealing with this type of arrogance and ignorance is taxing. If I fight
back, placing in the patient's chart the appropriate articles and writing notes
about legal risk if the best therapy is not employed, then I would win the
battle. The patient would receive the nutritional in question, and I will
have made an enemy. I would have the fight the same battle, with the same
people, with the next patient, and I would make more enemies. Retaliation
would follow, sometimes not just against me. I have sent the appropriate
articles to the hospital pharmacy and therapeutics committee and they would not
even respond. Thus I have given up. If you want to know why I
no longer personally manage my patients in the hospital, well now you know
(in contrast, when I was 35 and intellectually confined to what I had been
taught I was tied with two older guys as the leading cardiology admitter to my
then primary hospital - now I know better and can not confine myself to drug
only medicine). If I feel, based upon your symptoms, non-invasive work up,
and heart catheterization that your need CABG, then I will coordinate your
evaluation with a surgeon who I trust, and he will carry out the procedure.
Your post-operative care will include cardiologists who I trust (competent and
caring physicians who do not have my knowledge of nutritional medicine, such
that they don't get into these fights). I will receive feedback from all
involved prior to your 1st post-operative visit with me. We take great
care (and pride) in our ability to "hand off" your case, such that all bases are
covered.
The long term down side of CABG is the risk of graft closure. Our thin
walled veins are designed to convey deoxygenated blood in a non-pulsatile, low
pressure (5 mmHg) flow pattern back to the heart for reoxygenation. Placed
in the chest as a bypass conduit, we are asking them to carry oxygenated blood
in a pulsatile, high pressure (as high as your blood pressure) pattern.
This high pressure stress in a high oxygen environment places intense free
radical stress on the endothelial cells that line the vein graft.
Endothelial dysfunction (impaired production of nitric oxide) follows, the vein
walls become inflamed and they begin to fill up with plaque. The average
vein graft lasts seven years, but 1/3rd close off within one year. Some of
this is technical (if a vein graft is placed to a small artery it is more likely
to close off as flow within the vein graft will sludge and the graft will close
off), but much of vein graft disease is occurring on the basis of endothelial
dysfunction, something that we can address. So far, agents that improve
endothelial function in general, such as antioxidants, fish oil, the tissue
specific ACE inhibitor Quinapril, and the statin class of cholesterol lowering
drugs, have been shown to have favorable affects on vein graft patency and/or
post-CABG outcome. The best time to start endothelial preserving therapy
would be before your bypass surgery begins, continuing these agents within the
immediate post-bypass period (when your new vein grafts are exposed to excessive
free radical stress), but again, this type of logical therapy is not permitted
in our hospitals. Thus I will get you started on or started back on these
types of treatments as you recover. In contrast to vein grafts, the LIMA
and RIMA vessels are native arteries. They are used to high pressure, high
oxygen, pulsatile flow and their endothelial cells make a lot of nitric oxide.
So while half of all vein grafts close within 7 years, 90% of all arterial
grafts remain open at 10 years. Whenever possible, your heart surgeon will
utilize the LIMA (and often the RIMA as well) as bypass conduits for your CABG.
The technique of CABG is continually evolving, aiming to improve the
technical aspects of the procedure, such that your outcome is improved.
Two recent advances bear mention. Traditional "on pump" bypass was carried
out on a bloodless, arrested heart. Your heart would actually be stopped,
with your brain and other internal organs supplied by blood that was conveyed
through the bubble pump oxygenator. Tiny clots could form in the bubble
oxygenator and get stuck in your brain. This delayed your recovery from
CABG, and in extreme cases left you with impaired intellectual function.
Recent technical advances allow surgeons to operate "off pump", on a still
beating heart. The bubble pump oxygenator is no longer necessary, blood
flow to your brain is no longer impaired, and you recover much faster from the
procedure. "Off pump" CABG has been a major advance. Transmyocardial
laser revascularization, otherwise known as TMR, is the second major
breakthrough. If your surgeon places a vein graft to a small or diffusely
diseased (the whole vessel is full of plaque) coronary artery, flow through that
vein graft will be sluggish and the graft will likely fail. If all of your
arteries are small or diffusely diseased, you will be deemed "inoperable" and
you will be turned down for CABG. Your surgeon will not operate if the
procedure is obviously doomed to fail. But what if 1-2 of your arteries
could be grafted, but 1-2 are inoperable? Does the surgeon do 1/2 the job,
placing grafts to the operable vessels while ignoring the small ones? In
this situation you could easily experience a heart attack involving the heart
muscle served by the non-bypassed vessels. On the other hand, if he
doesn't operate, your chest pain will continue and you will eventually
experience a heart attack(s) on your own - what a dilemma! TMR allows
effective revascularization in this situation. Tiny channels are "drilled"
into the heart muscle with a medical laser. As the heart heals these laser
channels, a capillary blood supply will develop, and some degree of
revascularization will occur. TMR is typically not done as a stand alone
procedure (the results are not satisfactory when all three vascular
distributions are inoperable and TMR is used instead). TMR works great in
the situation where 1-2 vessels can be bypassed, and 1-2 cannot. TMR can
also serve as a bridge between CABG and EECP. I recall a patient with
severe angina and a poorly operable situation who underwent CABG combined with
TMR. Six months later he returned with more pain. I repeated his
angiogram and found two open and tow closed vein grafts. A heart attack
had not occurred, because his surgeon had carried out TMR on the heart muscle
supplied by the diffusely diseased arteries. The TMR effect was not strong
enough to keep the patient pain free, but it was enough to prevent a heat attack
when the two grafts failed. We had anticipated that the grafts to these
vessels might fail, so TMR was carried out concomitant to CABG. EECP was
carried out and the patient did great. EECP as a primary or initial
procedure would have failed, as all the vessels serving this patient's heart
were diseased. This program was actually planned out in advance by myself
and the heart surgeon who I work most closely with (wouldn't it be neat if I
could get the rest of his hospital to work with me - well maybe in 10 years)!
.
 end
is sewn into a diseased coronary artery, beyond its point of blockage,
"bypassing" the blockage. Oxygenated blood is thus resupplied to a
previously oxygen starved region of heart muscle. Energy production will
normalize and your symptoms will resolve. Whenever possible, surgeons will
utilize arterial grafts during CABG. The left internal mammary artery
originates from the left subclavian artery (which goes on to supply the left
upper extremity). The left internal mammary artery (LIMA) normally
provides oxygenated blood to the left upper chest wall. When used as a
bypass conduit, the proximal end of the LIMA is left attached to the left
subclavian artery. The small side branches given off the LIMA to supply
the chest wall musculature are tied off. The distal end of the LIMA is
mobilized away from the chest wall and is then sewn into a coronary artery,
usually the left anterior descending (LAD), "bypassing" the blockage.
Blood flow will take the path of least resistance, so following bypass surgery
the narrowing in the diseased but now bypassed native artery will often close,
but that is not an issue, as the wide open graft will supply all the oxygenated
blood that is required. The superficial leg veins were designed to
transport deoxygenated, or "used" blood from the cells of the leg back to the
heart, for later re-oxygenation as the used blood flows through the lungs.
The superficial leg veins are actually responsible for only 15% of lower
extremity return blood flow. The deep veins are responsible for the
other 85%. They are left intact, so ankle swelling is typically not a
problem following CABG in young people. Older patients may need to wear
support stockings following bypass surgery, but this is not a huge price to pay.
The real problem with vein grafts is that we are asking a vein to do an artery's
job (more on this later). The chest wall also receives arterial blood from
vessels that originate in the abdomen. Following bypass surgery that
utilizes the LIMA, patients often note a vague discomfort over the chest wall.
This sensation is sometimes difficult to differentiate from your prior angina,
because it is mild "angina" of the chest wall, as it's blood supply has been
reduced. This is not a threat and the discomfort is only minor, and is not
a cause of worry.
end
is sewn into a diseased coronary artery, beyond its point of blockage,
"bypassing" the blockage. Oxygenated blood is thus resupplied to a
previously oxygen starved region of heart muscle. Energy production will
normalize and your symptoms will resolve. Whenever possible, surgeons will
utilize arterial grafts during CABG. The left internal mammary artery
originates from the left subclavian artery (which goes on to supply the left
upper extremity). The left internal mammary artery (LIMA) normally
provides oxygenated blood to the left upper chest wall. When used as a
bypass conduit, the proximal end of the LIMA is left attached to the left
subclavian artery. The small side branches given off the LIMA to supply
the chest wall musculature are tied off. The distal end of the LIMA is
mobilized away from the chest wall and is then sewn into a coronary artery,
usually the left anterior descending (LAD), "bypassing" the blockage.
Blood flow will take the path of least resistance, so following bypass surgery
the narrowing in the diseased but now bypassed native artery will often close,
but that is not an issue, as the wide open graft will supply all the oxygenated
blood that is required. The superficial leg veins were designed to
transport deoxygenated, or "used" blood from the cells of the leg back to the
heart, for later re-oxygenation as the used blood flows through the lungs.
The superficial leg veins are actually responsible for only 15% of lower
extremity return blood flow. The deep veins are responsible for the
other 85%. They are left intact, so ankle swelling is typically not a
problem following CABG in young people. Older patients may need to wear
support stockings following bypass surgery, but this is not a huge price to pay.
The real problem with vein grafts is that we are asking a vein to do an artery's
job (more on this later). The chest wall also receives arterial blood from
vessels that originate in the abdomen. Following bypass surgery that
utilizes the LIMA, patients often note a vague discomfort over the chest wall.
This sensation is sometimes difficult to differentiate from your prior angina,
because it is mild "angina" of the chest wall, as it's blood supply has been
reduced. This is not a threat and the discomfort is only minor, and is not
a cause of worry.