Return to Treatments Available Page
Dual-Chamber Pacemaker Implantation for CHF
You might think that a nutritionally oriented cardiologist would be against implanting a computerized pacing device into your body. I'm not. I would prefer to turn your heart around with MME, detoxification, EECP, and nutritional interventions, but if these alone do not get the job done, or if these approaches are not possible (because your insurance will not cover them), then I will recommend that you be considered for dual-chamber pacing/defibrillator placement.
The damaged, dilated heart often develops a conduction disturbance. The wiring that carries the electrical impulse from the pacemaker cells to the heart muscle cells becomes frayed. On your EKG this manifests itself as an "intraventricular conduction delay" or "bundle branch block". This means that the cells in one wall of your heart are activating a little before the cells in another wall of your heart - the heart is no longer contracting in a synchronous fashion. If one wall squeezes in while another wall is squeezing out, cardiac function will fall. Ejection fraction will fall, as the heart is not able to pump out as much blood, and the filling pressure within the heart may rise, which you experience as shortness of breath. The heart may enlarge further, valve function may falter, and the conduction delay might even worsen as a result.
Thus this conduction delay, this dysynergy in cardiac wall motion, is both a consequence, and a cause, of CHF. The correction, dual chamber pacing, is theoretically simple, while the engineering that made it possible is complex.
Standard pacemaker therapy, designed only to maintain the heart rate at a certain minimum level, involves placing a single pacing wire into the right ventricle, via the subclavian vein (located beneath the collar bone). A small incision is made in the armpit to allow placement of the pacemaker software and battery, which is similar in size to a cigarette lighter.
Standard, ventricular pacing can leave the ventricles, the pumping chambers, out of synchrony with the atria, the pump priming chambers. About fifteen years ago the concept of AV (atrial-ventricular) pacing came out. Here, two separate wires are placed within the subclavian vein. One is advanced into the right ventricle, and one into the right atria. The pacemaker software allows for the atrial pacemaker lead to fire a half second of so before the ventricle is activated. This AV pacing maintains atrial priming of the ventricular pump. The result is better overall cardiac function - this was a major advance.
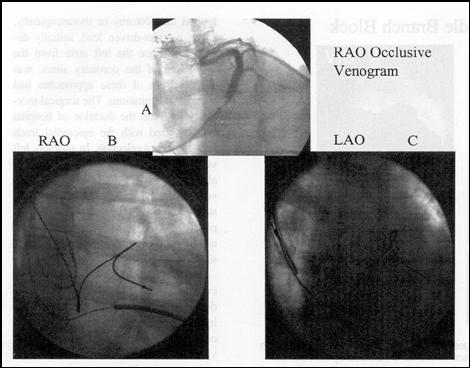
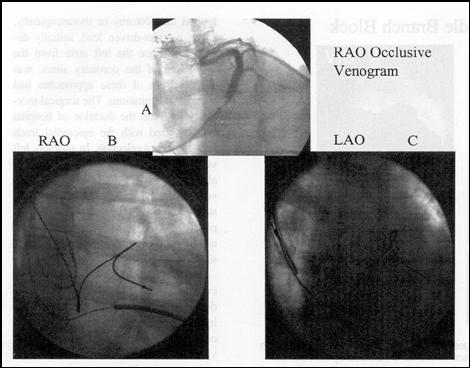
Dual-chamber pacing is even better. Here pacing leads are advanced into the right heart chambers, and another lead is advanced into the vein that drains the left heart. A pacing stimulus at this location will activate the left ventricle, but not the right ventricle. The software allows for adjustment in the pacing rate of all three wires. If an intraventricular conduction delay is delaying activation of one wall of the left ventricle, then it can be electrically activated a split second earlier than is the opposite wall. If a delay between activation of the atria and activation of the ventricles is adversely affecting closure of the valves of the heart, this can be corrected as well. All of these adjustments can be carried out non-invasively, with a telemetry unit supplied by the manufacturer. Several studies have documented benefit of dual-chamber pacing in the patient with CHF and an intraventricular conduction delay.
The graphics below contain findings from three studies. Following placement of a dual chamber pacing device, ejection fraction rises slightly, the cardiac chambers decrease in size, and functional status improves (NYHA functional class falls, and six minute walking distance increases).
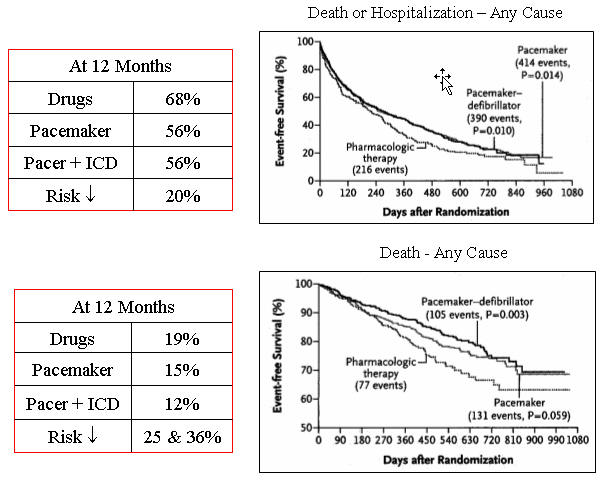
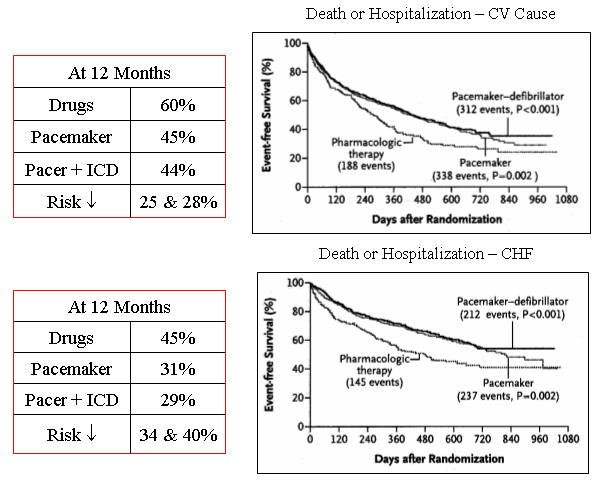
Patients with advanced CHF are just as likely to die from a cardiac rhythm disturbance as they are to die from pump failure. Thus if we are going to put in a dual chamber pacemaker, a case could be made for adding in a defibrillator capability (the hardware is basically the same). The study abstracted below compared dual chamber pacing with defibrillator capability vs. dual chamber pacing alone vs. continued drug therapy alone in 1520 patients with advanced CHF (ejection fraction £ 35%), all on optimal drug therapy going in to the study.
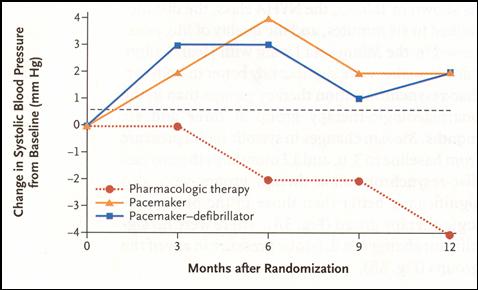
Patients in this condition typically have a low systolic blood pressure, due to the pump dysfunction present and the drugs required to keep them out of overt CHF. This low systolic blood pressure is associated with fatigue. Over the 12 months following device placement, systolic blood pressure rose slightly in both pacing groups, and fell further in the continued drug therapy alone group.
Six minute walking distance and the Minnesota heart failure score, measures of functional status, also improved more in the dual chamber paced patients.
The charts below describe rates of death and death or hospitalization from any cause and from a cardiovascular cause. You can see that in all categories, dual chamber pacing was superior to continued drug therapy alone. With respect to all cause mortality, the pacing + defibrillator group did a little better than the pacing alone group. Therefore, the current practice, in a patient with CHF, pump dysfunction, and an intraventricular conduction delay, is to place a pacing device that allows for dual chamber AV pacing with defibrillator capability. Many of my patients have received these devices, and I have been impressed with the results. Effort capacity improves, and in many cases, ejection fraction rises in an obvious fashion. The down side of dual chamber pacemaker placement is that it closes the door forever to MME. The upside is that it works, and that it is covered by Medicare
James C. Roberts MD FACC
1/01/07