Return to Medical Topics Home Page
Return to CHC Home Page
HMG-Co-A Reductase Inhibition
Statin Drugs - Saviors or Satins?
Should you take a statin? Allopathic Medicine* is pushing you to do so, and here, Allopathic Medicine has a point. Statin drugs (HMG Co-A Reductase Inhibitors) lower LDL cholesterol, attenuate oxidative and inflammatory stress, and improve endothelial function. Clinical trials demonstrate consistent benefit of HMG Co-A Reductase Inhibition in the treatment of CV disease states, with less powerful primary prevention benefits. If you are hospitalized with a CV disorder, statin therapy will likely be added, irrespective of you baseline LDL cholesterol, even if your arteries are wide open. Your position here will not matter (because “it’s the standard of care”). Many of you don’t like this.
Integrative Practioners are being cajoled and heckled for not putting you on these agents if you have CV disease or if your cholesterol is “not at target”. While I can ignore administratively threatening and repetitive letters from insurance companies, practitioners under the age of 40 cannot (what will happen if they drop me; what if I lose my referral sources)? MDs/DOs in mega-groups (the rule these days) have little choice but to go along with the group position; otherwise they will be bullied to comply (or fired).
I don’t like this pressure, no more than I appreciated the criticism I received 30+ years ago for prescribing Lovastatin (I trained at the right place and understood this approach early on) to treat what was then “mild” hyperlipidemia (cholesterol 300-325 mg/dl).
Allopathic Medicine down plays the down side of statin therapy, while my professional colleagues and friends (see The STATIN Disaster, by David Brownstein MD, and The Great Cholesterol Myth, by Stephen Sinatra MD) raise concern regarding statin side-effects and question their across-the-board utilization.
What should you do? What will I recommend when I see patients who are also working with Drs. Brownstein and Sinatra? Also, if you take a statin, should you supplement with the key nutrients that statins deplete (your MDs/DOs will likely tell you that “vitamins don’t work”)?
These questions can be best answered if we review the role of HMG Co-A Reductase in atherosclerosis, keeping in mind that atherosclerosis (an interaction between cholesterol and oxidative and inflammatory stress) is a maladaptive response of the immune system to what it perceives as infection of the artery wall with oxidized lipids (this concept is discussed in greater detail on our recent UTube presentations and in the Oxidative Stress in Atherosclerosis write-up on Heartfixer.com).
*(MDs/DOs confined to FDA approved invasive/ pharmaceutical interventions, corresponding professional societies, insurance companies, and the pharmaceutical industry
The Hyperlipidemia of Pseudo-Infection
In response to legitimate infection, HMG-Co-A Reductase (the rate-limiting step in cholesterol generation) upregulates (increases its activity). This makes sense, as you need cholesterol to manufacture cell membranes for the rapidly proliferating white blood cell defenders. It also helps if you can activate the endothelium, making it easier for the defenders to access infected tissues, and to generate ROS/RNS (reactive oxygen and nitrogen species, otherwise termed “free radicals”) bullets to kill the microbes.
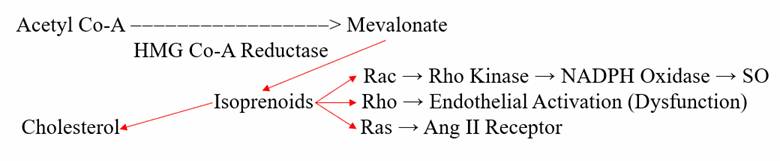
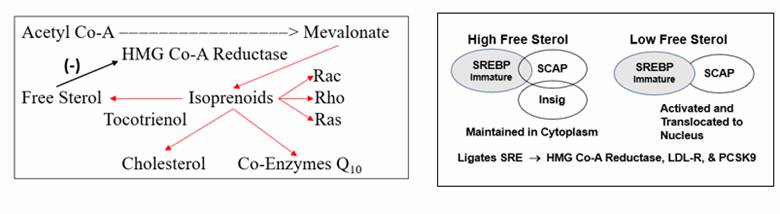
HMG Co-A Reductase generates cholesterol through a system of intermediate molecules, including the isoprenoids farnesyl and geranylgeranyl pyrophosphate. They activate the signaling molecules Rac, Rho, and Ras, which in turn upregulate superoxide free radical production (bullets to kill microbes), activate the endothelium (to allow responding white blood cells easy access to the microbes), and up regulate Angiotensin II receptor expression (more free radical production and more endothelial activation). Superoxide overload in turn promotes NF-kB translocation (our primary infection sensing inflammation up regulation pathway), to generate more pro-inflammatory cytokines (a virtuous cycle to deal with infection).
This system worked great for primitive man. Genomic hyperlipidemia thus arose as a defense against perinatal sepsis, the leading cause of death in the history of mankind. A minority of us carry these traits, accounting for the infrequently encountered situation of familial hyperlipidemia (good for your ancestors but bad for you). As a corollary, if your bear sickle cell genes you will not die of malaria (Mother Nature never does anything without a good reason).
In the rest of us HMG Co-A Reductase is not genomically up regulated, and when we are young our cholesterol levels are low. However, in Western Man, cholesterol values start to rise in our 20s, and continue to rise with aging. Why is this occurring? What factors determine the level of expression of HMG Co-A Reductase? Also, in legitimate infection, how does the enzyme know to up regulate? What are the triggers?
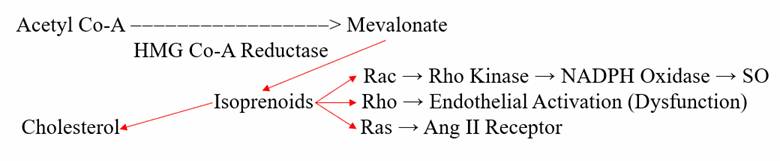
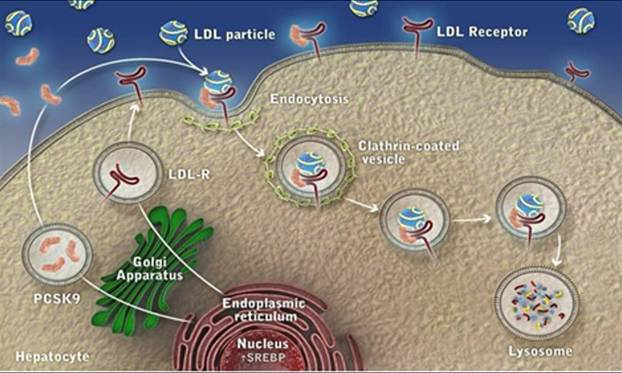
HMG-Co-A Reductase expression (level of enzyme activity) is governed by the cell’s perceived need for free cholesterol. When intracellular free cholesterol is adequate, the free cholesterol sensor Insig sequesters SREBP (Sterol Regulating Element Binding Protein) within the Endoplasmic Reticulum. When free cholesterol is low, Insig releases SCAP (Sterol Regulating Element Binding Protein Cleavage Activating Protein) to transport SREBP to the Golgi apparatus, where it is enzymatically modified, promoting its translocation into the nucleus, where it binds the Sterol Regulator Element (SRE), the promoter site for HMG Co-A Reductase (the rate limiting step in cholesterol generation). Biochemistry aside, this cholesterol thermostat system allows for generation of cholesterol only when it is needed. When free cholesterol is perceived to be adequate or in excess, cholesterol generation stands down – that is Mother Nature’s rule. But if this is Mother Nature’s rule, why are our patients overproducing cholesterol even when their cholesterol levels are rising (this key question will be answered below)?
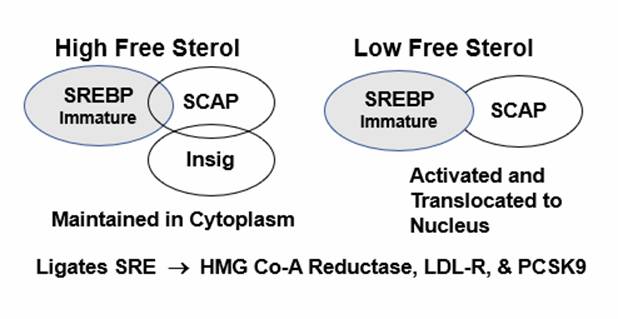
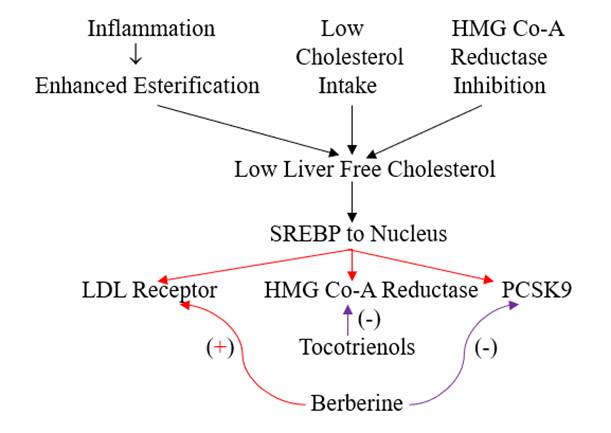
Activation of the SRE within liver cells (when intracellular free cholesterol is low) leads to transcription** of the LDL receptor protein, enabling the liver cell (hepatocyte) to pull more cholesterol out of the circulation. This is the clinical goal of statin therapy. If we inhibit HMG Co-A Reductase (what statins do), liver intracellular free cholesterol falls, SCAP will then escort SREBP to the nucleus, it binds the SRE, LDL receptors are elaborated, and the liver then pulls cholesterol out of the circulation. Thus, your serum LDL level falls.
However, from the LDL control perspective, while statins do one good thing (stimulate the transcription of LDL receptors), they also do two bad things, setting the biochemical stage for statin breakthrough and recurrent hyperlipidemia.
The Insig/SCAP/SREBP/SRE cholesterol thermostat system was not created to make us good statin takers. Rather it was created to ensure that Primitive Man did not become cholesterol deficient when dietary cholesterol intake was limited. Thus, SRE activation (due to low liver intracellular cholesterol) also leads to transcription of more HMG Co-A Reductase (if cholesterol is low, why not make more)?
Cholesterol biosynthesis and uptake occurs mainly in the liver, and as Mother Nature doesn’t want the liver to hog all the cholesterol, SRE activation also leads to the generation of PCSK9 (Proprotein Convertase Subtilisin/Kexin type 9), a counterbalancing protein that degrades the hepatic LDL receptor, maintaining serum cholesterol to meet the needs of other cells.
PCSK9
Degrades the LDL Receptor
®Blunts
return of LDL to the liver
®Raises
circulating LDL
Expression increased by Inflammatory Cytokines
So, from the perspective of cholesterol reduction, statins do one good thing (generate more LDL receptors to pull cholesterol out of the circulation) and two bad things (generate more HMG Co-A Reductase and more PCSK9). Stated otherwise, statin mono-therapy sets the stage for its failure. Your LDL falls with initial therapy, but 6-12 months later it may be back up. Initially I attributed this to complacency on your part; your LDL fell so you loosened up on your diet. Complacency may play a role, but biochemically the reason for “statin escape” is upregulated generation of HMG Co-A Reductase and PCSK9. Have you ever been told that statin drugs actually increase the generation of the enzyme that they inhibit?
We respond to statin escape by increasing your statin dose. When this doesn’t work, we add ezetimibe, which blunts cholesterol absorption in the small intestine (mimicking the effects of a low cholesterol diet). You are now on two drugs, with your statin at a high dose. If this doesn’t work, we add in twice a month injection with a PCSK9 inhibitor (this works very well but is quite expensive). Integrative Cardiology offers you a different plan (to be presented below), a plan based upon an understanding of human physiology (not drug adds and insurance mandates).
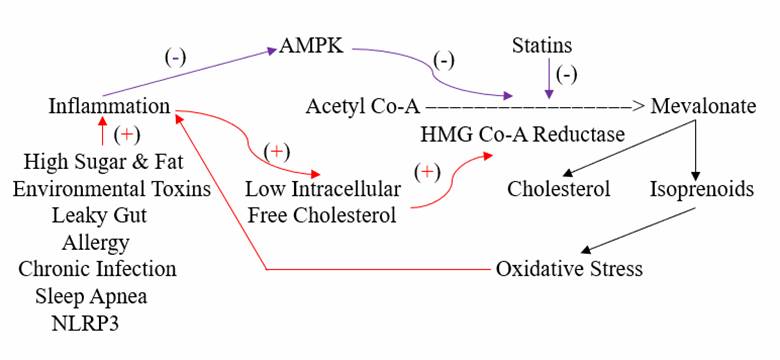
Inflammation Mimics Infection and Increases Cholesterol Generation
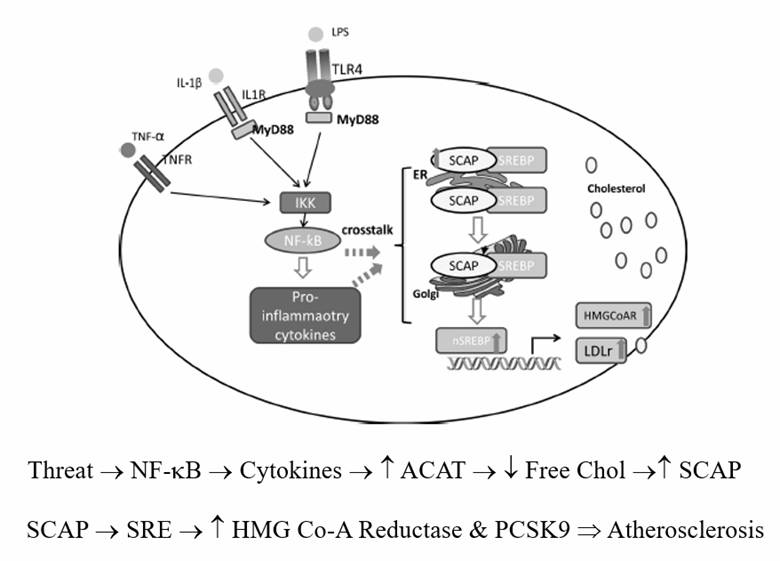
In the presence of legitimate infection (lipopolysaccharide) or inflammation (pro-inflammatory cytokines such as TNF-a or Il-1b), Acetyl Co-A Acyl Transferase (ACAT) expression up regulates, promoting cholesterol esterification (binding a free fatty acid to cholesterol, to store up these key raw materials for the upcoming infectious winter). As hepatocyte cholesterol esterification proceeds, free cholesterol falls, and as Insig senses only free cholesterol, HMG Co-A Reductase and PCSK9 transcription increase, even though total intracellular cholesterol is rising.
In Western Man, not in relation to real infection, intracellular and circulating cholesterol rise with age. This doesn’t relate directly to dietary cholesterol (in our 20s we consumed pizza, burgers, and beer and our cholesterol values were low) but rather to the progressive accumulation of infection mimicking pro-oxidant and pro-inflammatory phenomena (visceral fat, leaky gut, metals, organic pollutants, etc.) that lead to maladaptive and progressive HMG Co-A Reductase and PCSK9 transcription.
Avoiding or resolving the age and diet related oxidative/inflammatory cues that increase HMG Co-A Reductase transcription is the best approach here. But if the patient is unable or unwilling to take these steps, or if we do not have the luxury of time (you just experienced a heart attack due to bypass graft failure and your CRP is 10 and your oxidized LDL is100), then interventions to inhibit HMG Co-A Reductase activity to lower cholesterol and reduce trafficking through the NOX, ATR1, and NF-kB pathways (blunting oxidative and inflammatory stress; blunting the “pseudo infection” signaling that drives atherosclerosis) makes sense. This can be expeditiously achieved with statin drugs, which function as “competitive inhibitors” of HMG Co-A Reductase. These agents look like HMG Co-A (two Acetyl-Co-A molecules bound together), the molecule that HMG Co-A Reductase converts into mevalonate. Statins instead bind to and inhibit the enzyme (the wrong key that gets stuck in the lock), blocking mevalonate generation in a dose-dependent fashion (that is until more HMG Co-A Reductase is generated, as you now know to be an undesirable effect of statin drugs).
The indication for blunting biochemical trafficking through the HMG Co-A reductase pathway is not a specific cholesterol level, but rather the presence of inflammation and oxidative stress in the presence of atherosclerosis, endothelial dysfunction, or other factors suggesting that inappropriate HMG Co-A Reductase up regulation may cause clinical harm. There will be little gain in 30-year-old women with an LDL of 130 and an otherwise pristine risk profile, but tremendous gain in her diabese grandfather who sustained his second MI due to graft failure, whose LDL is at a similar level.
HMG Co-A Reductase is also a key step in the generation of a number of critical molecules, all of which are knocked down with statin therapy.
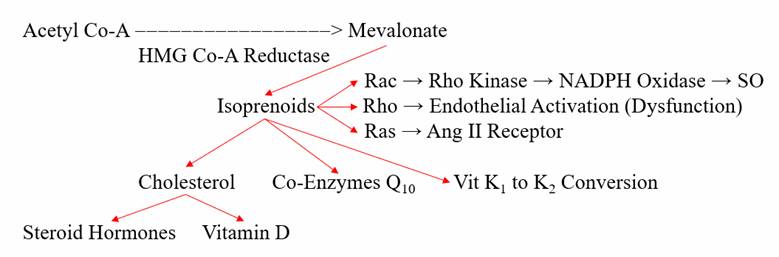
We need cholesterol to generate cell membranes, steroid hormones, Co-Enzyme Q, the transfer RNA involved in selenomethionine (immune and antioxidant enzyme function), and the enzyme needed to convert K1 in to K2 (K2 prevents vascular calcification). Thus, overly aggressive statin therapy will compromise key aspects of our health. Co-Q deficiency compromises energy generation and leads to weight gain and impaired cardiac energy generation (even low dose statin therapy without Co-Enzyme Q supplementation leads to diastolic dysfunction, essentially a “stiff heart”). Loss of testosterone leads to inflammation, fatigue, and reduced protection against auto-immunity (and something that should be stiff becomes less stiff); but never mind – it’s the “standard of care”. Statin therapy accelerates vascular calcification. Muscle pain, depression, impaired cognition, and a deterioration in insulin sensitivity may occur (so we add in other drugs to deal with these conditions that we created). Can you see why Drs. Sinatra and Brownstein feel this is a little bit insane?
Do TV adds talk about this? Do your other Doctors tell you about this? Apparently, we are supposed to be compliant pill takes and accept these side-effects so we can achieve a “target LDL level”. American Doctors no longer tell you not to take Co-Enzyme Q, but that is because chain drug store adds tell us that their brand of Co-Enzyme Q is the one most recommended by Cardiologists (if it’s on TV than Doctors will go along).
Within our framework of Integrative Cardiology (understanding how our body works and how we can influence its function with drug and non-drug approaches,, we can obtain the benefits of HMG Co-A Reductase inhibition while attenuating its side effects. First of all, if we give you a drug that leads to nutritional deficiency, it is only appropriate to replete the nutrients knocked out. Thus, if you are taking a statin it is reasonable (and really biologically responsible) to supplement with Co-Enzyme Q10 (and here we can obtain levels), Vitamin D, and Vitamin K2. If testosterone falls significantly, the (non-oral) bioidentical testosterone replace therapy makes sense.
As “prevention” in Allopathic Medicine is confined to statins and other drugs, many important bases are not covered, and thus the tendency to maximize the dose of the drugs we do employ. Now, if HMG Co-A Reductase is inappropriately up regulated, inhibiting enzyme activity back to the level found in a healthier you, say an age 25 you, makes sense. We don’t do this. We don’t know what your cholesterol was when you were 25, we just put you on statins (and later, due to the statin escape phenomena that you now understand, we increase the dose and later add in other drugs). Within the paradigm of Integrative Cardiology, we go after every cause of atherosclerosis that we are aware of. Thus (my position) we can keep you out of trouble with less severe inhibition of HMG Co-A to mevalonate conversion. Please take note of my choice of words. The goal is not to take a statin but rather to inhibit mevalonate production and isoprenoid pro-oxidant and pro-inflammatory signaling, while optimizing liver cell membrane LDL receptor expression.
Enzyme activity (often referred to as expression) is physiologically regulated
at four levels:
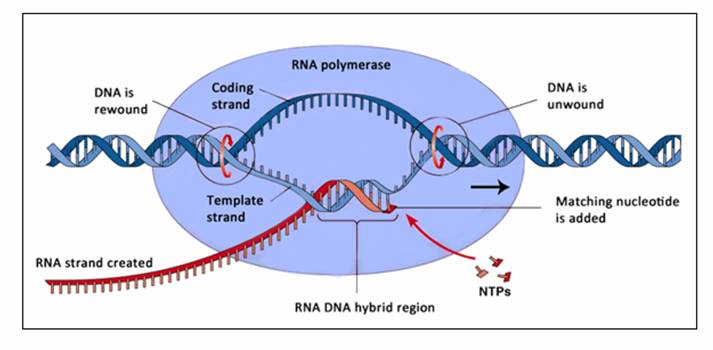
A. Transcription** – A transcription factor (here SREBP) translocates (travels
from the cytoplasm, the non-nuclear cell fluid) in to the nucleus (which
contains the DNA template), binds to a promoter (a transcription “start sign”,
here the SRE) and then copies the DNA message (genetic code) on to a mRNA
(messenger RNA molecule).
B. Translation – The mRNA molecule returns to the cytoplasm, where the genetic
information is translated into a chain of amino acids that make up a structural
protein or an enzyme (in this discussion HMG Co-A Reductase).
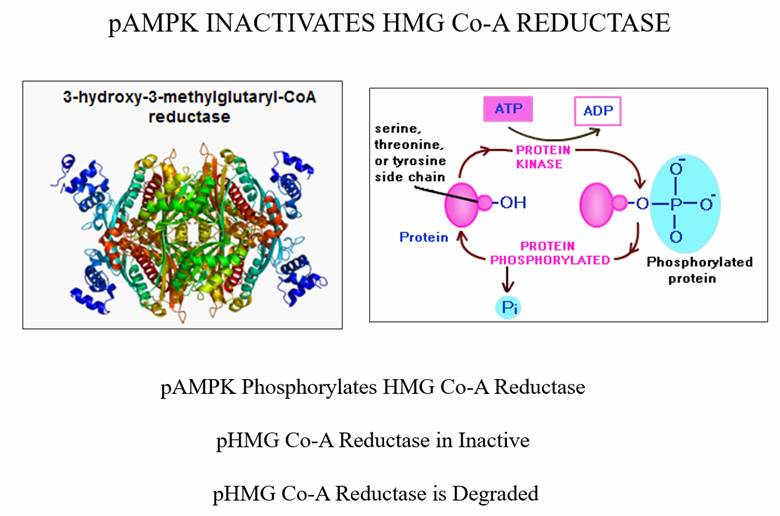
C. Post-translational regulation – As conditions within the cell fluid change,
it is important that we be able to respond rapidly by turning up or turning down
a specific enzyme, and we do this by adding or removing a phosphate group from
specific sites within an enzyme. AMPK (AMP Sensitive Protein Kinase – up
regulated by berberine) phosphorylates HMG Co-A Reductase, turning down its
activity, and marking it for ubiquination.
D. Ubiquination – This process degrades “old” enzymes in to its component amino
acids. Ubiquination may also be up regulated if the body senses a need to
decrease the expression of an enzyme (this step in not related to Co-Enzyme Q,
which is sometimes referred to as ubiquinone). Tocotrienols promote HMG Co-A
Reductase ubiquination and hence degradation.
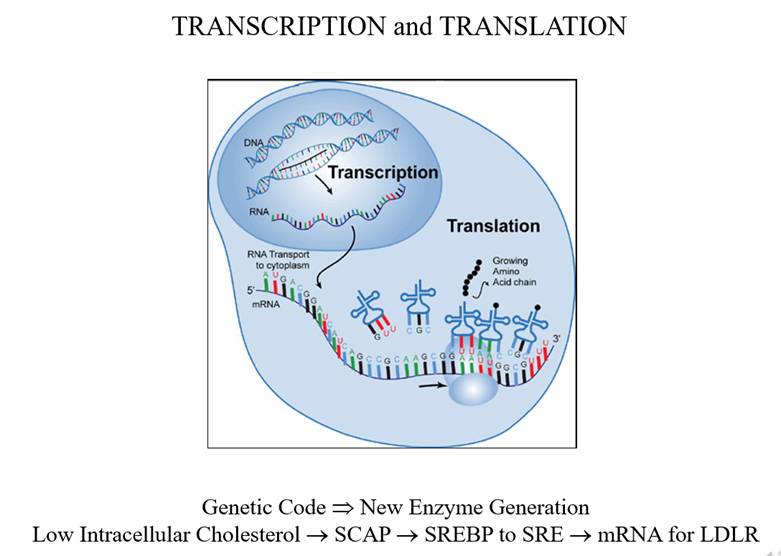
Translation of mRNA into LDL Receptor protein
Post-Translational Modification. AMPK is activated (phosphorylated) by exercise, weight loss, berberine, and any other phenomena that lowers oxidative and inflammatory stress burden. Conversely, inflammatory stimuli (the same culprits that promote inappropriate cholesterol esterification leading to increased cholesterol generation) down regulate AMPK activity.
Statin drugs (and non-pharmaceutical HMG Co-A Reductase inhibitors, which will be discussed later) do not work directly at any of these steps. They are not part of Mother Nature’s plan – all they do is inhibit (essentially therapeutic poisoning) the HMG Co-A Reductase enzyme.
Within the framework of Integrative Cardiology we can influence HMG Co-A Reductase expression by working at all levels of enzyme control.
Berberine up regulates expression of AMPK (as
does exercise, caloric restriction, and other dietary/lifestyle factors that
lower inflammation). Thus, Berberine leads to HMG Co-A Reductase
phosphorylation, with subsequent enzyme inhibition. The mRNA for the LDL
receptor is relatively delicate; much is degraded before it can be translated
into the active enzyme. Berberine stabilizes LDL receptor mRNA fragments. Thus,
more is translated, membrane LDL receptor expression increases, more cholesterol
returns to the liver, and thus your LDL levels will further decrease.
Recall that SREBP activation leads not just to more LDL receptor mRNA (desirable
if the goal is to lower LDL) but also more HMG Co-A Reductase (undesirable) and
more PCSK9 (really undesirable, as PCSK degrades the LDL receptor protein).
Berberine blunts transcription of PCSK9. Stated otherwise, berberine will
synergize with drug (statin) and non-drug HMG Co-A Reductase inhibition, leading
to lower LDL values, less inflammation, and less oxidative stress. Berberine
thus goes a long way towards preventing the “statin escape” phenomena. Insulin
insensitivity occurs as a side-effect of statin therapy. Your glucose levels
will rise a little. We are supposed to ignore this phenomenon and rationalize
that the LDL lowering benefit out ways the drug-induced impairment in glucose
control. Berberine directly enhances insulin receptor expression and blunts
insulin insensitivity on the basis of inflammation, another reason to take
berberine whenever HMG Co-A Reductase inhibition is being utilized. Berberine
is discussed in great detail in our UTube presentations The Chronicles of
Berberine (click Audio-Visual Presentations on the Heartfixer.com home page).
Tocotrienols differ from Tocopherols (Vitamin Es) in that they bear an unsaturated double bond in their side-chain. This renders tocotrienols more mobile within the cell membrane, greatly enhancing their antioxidant effects. Tocotrienols also convert isoprenoid molecules (the intermediates in cholesterol generation that activate the pro-oxidative and pro-inflammatory Rac, Rho, and Ras pathways) in to free sterols. As free sterols rise, SREBP sequesters within the endoplasmic reticulum, and HMG Co-A Reductase transcription is blunted. Also, tocotrienols promote ubiquination (and thus degradation) of HMG Co-A Reductase molecule.
Thus, within the framework of Integrative cardiology, we can utilize a statin drug at a low dose (or utilized a nutraceutical HMG Co-A Reductase inhibitor), along with berberine and a tocotrienol, and obtain significant LDL reduction, with less downstream nutrient wasting and a beneficial as opposed to adverse effect on glucose metabolism.
Red Yeast Rice Extract (RYRE) contains a small amount of Lovastatin (the first prescription statin utilized 30+ years ago) and larger amounts of a related substance (Monocolin K). RYRE competitively inhibits HMG Co-A Reductase, providing physiologic effects qualitatively identical to those of statin pharmaceuticals. As RYRE is plant-based, the liver readily breaks it down, and statin drug side-effects (muscle pain, cognitive impairment, and ED) are less frequently encountered. In China RYRE is a standard therapy and has been shown to lower post-heart attack recurrent event risk at a level similar to that of stain drugs in the West. RYRE is an extract obtained from Red Yeast (Monascus purpureus) grown on rice. Yeast is not present in the RYRE supplement itself. The starting dose of RYRE is 600 mg twice a day, to be advanced, as needed, up to 2400 mg twice a day.
Bergamot is extracted from a fruit that grows best in Southern Italy. European research demonstrates that Bergamot 500 mg twice a day works as well as 10 mg/day Rosuvastatin, and that 1000 mg of Bergamot plus 10 mg of Rosuvastatin works as well as 20 mg of Rosuvastatin. Bergamot has been shown to be well tolerated in statin-sensitive patients. While Bergamot works well in the European studies, I don’t see it working well in my patients. It may be that the quality of Bergamot that we can get in the US is sub-par. Hopefully better Bergamot will become available but for now Bergamot is a second-tier choice.
Amla, extracted from the fruit Emblica Officinalis, inhibits HMG Co-A Reductase and lowers LDL and CRP, will raising HDL and improving insulin sensitivity. 500 mg of Amla worked as well as 20 mg of Simvastatin. Curiously, 500 mg may work better than 1000 mg. Amla, RYRE, Tocotrienols, and Bergamot, and the studies that support their use, are discussed in our UTube presentation Integrative Cardiology for the Chelation Physician – Part Five.
What is an optimal cholesterol? What should be your personal goal? This depends, of course, on the status of your arteries and your overall health. If you are 70 and your arteries are normal I don’t much care about your LDL level, but I care a lot if you are 40 and bear carotid plaque. Integrative Cardiologists like myself can make recommendations based on an assessment of your current arterial health (Carotid Artery Intima-Media and Endothelial Function), in relation to your overall health and non-lipid risk factors.
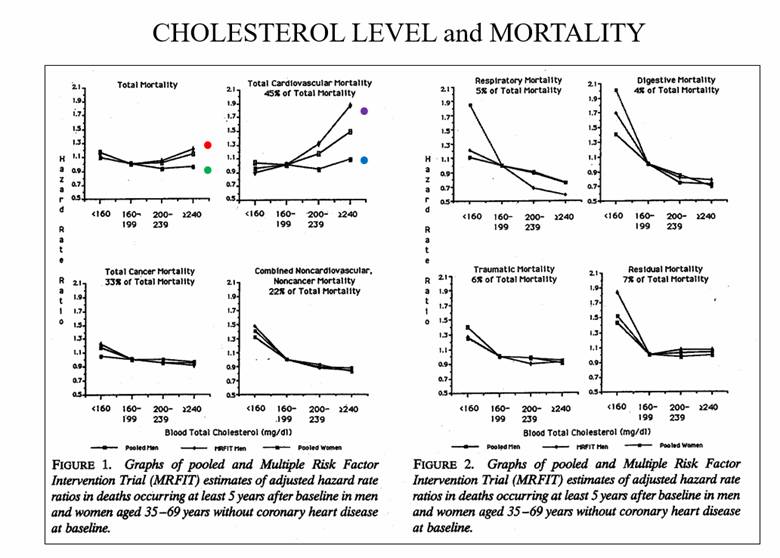
Epidemiologic studies tell us that in healthy individuals, 15-year mortality is lowest with a total cholesterol in the 160-200 range. Above 200 CV mortality rises in men but not in women. Below 160 mortality increases in both genders (particularly suicide, motor vehicle accidents, and cancer death). This data refers to overtly healthy individuals. This data does not mean that we are increasing your risk if we lower cholesterol below 160 in individuals with known CV disease.
If you and your Physician feel that LDL
reduction is appropriate, along with the common sense diet/lifestyle/weight
loss/detoxification measures outlined above, what interventional steps can be
taken?
1. HMG Co-A Reductase down-regulation:
a) Statin drugs are inexpensive and easy to take. My preference is Rosuvastatin,
starting at 5 mg every other day, slowly increasing the dose to achieve an LDL
appropriate for the individual, while watching for statin-related side-effects.
SLCO1B1 is a liver enzyme that metabolizes many of the statin agents. If you are
genomically down regulated for SLCO1B1, than you should have less trouble with
Rosuvastatin, Pravastatin, and Fluvastatin in comparison to the other agents
available.
b) Nutraceutical HMG Co-A Reductase inhibitors consist of:
a) RYRE,
starting at 600 mg twice a day, increasing as needed to 2400 mg twice a day.
b) Amla,
starting at 500 mg daily and increasing, if needed, to 500 mg twice a day.
g)
Bergamot 500 mg twice a day.
c) Berberine 500-1000 mg twice a day to synergize with drug and non-drug
approaches.
d) Tocotrienol supplementation can be added in if LDL reduction is not optimal
and/or if evidence of oxidative stress exists.
Concomitant use of berberine and a tocotrienol allows us to get the job done with lower doses of any HMG Co-A Reductase inhibitor, while providing additional attenuation of insulin insensitivity and oxidative and inflammatory stress, a common sense approach that is backed up with clinical trials (that will not be presented to you on TV ads).
e) Repletion of key nutrients wasted by HMG
Co-A Reductase inhibition. This will occur with statin drugs, and may also
occur if we push with the nutraceutical HMG Co-A Reductase inhibitors. Thus,
repletion makes sense, especially as these molecules themselves are
preventive/therapeutic in many CV conditions:
a)
Co-Enzyme Q 100 mg/day should accompany HMG Co-A Reductase therapy, or we can
measure Co-Q and supplement to maintain an appropriate level. In healthy
individuals, a normal reference range value is OK, while individuals with
coronary insufficiency and heart failure do best with a level
³
2.5. I take Designs for Health Q-Evail 100 mg on a daily basis.
b) The
American diet is low in K2 (obtained from meat and dairy if the animals eat
grass; the animals we eat are fed corn and soy bean). K2 deficiency contributes
to vascular calcification, statins waste K2, and increased vascular
calcification accompanies statin therapy. 100 mcg/day of K2 makes sense if you
are taking a nutraceutical statin or as a general preventive, while 1000 mcg/day
is appropriate is you bear vascular calcification or if you are taking a drug
statin. K2 is protective against osteoporosis and has been used in the treatment
of bone marrow and liver malignancies. We cannot measure Vit K at present, but
there is no down side to intake of up to 35 mg/day. K2 does not promote blood
clotting, but if you take Warfarin (Coumadin) it is inadvisable to take K2***.
Warfarin works by blocking the recycling of K1, which is needed to make clotting
factors. K2 can be converted into K1, necessitating an increase in your
warfarin dose (K2 is discussed in
Integrative Cardiology for the Chelation Physician - Part Three).
*** Other
practioners advise taking K2 and increasing
your Warfarin dose to compensate for the K1 that is derived from K2 but I feel
this plan has more downsides than upside.
g) Steroid hormone generation is compromised by statin therapy. Physiologic testosterone is protective against CV disease in men. When we knock out testosterone with stain drugs, you experience fatigue, depression, and inflammation – basically you feel knocked out. Thus we can measure testosterone and estradiol, and take appropriate corrective action (please see our Testosterone – The Heart Hormone for Men UTube presentation).
d) Vitamin D deficiency is the rule in un-supplemented Americans (wheat germ agglutinin in our diet may be the culprit). Whether you are or are not taking a stain, get your level measured, and supplement to get above 30, and ideally in the 50-60 range (some practitioners recommend higher levels).
e) Selenomethionine is the form in which our physiology utilizes selenium in the generation of antioxidant and other defense enzymes. The tRNA molecule involved in selenomethionine utilization is knocked out with statin therapy. This may be part of the mechanism of benefit of statin therapy, in that in atherosclerosis immune overactivity is a driving force. Multiple studies have looked for synergy between statins and antioxidant supplementation. The only supplement that had a negative effect was selenium (one study). As maladaptive immune overactivity is a driving force in atherosclerosis, compromising immune function by knocking out selenium nutriture may be a means through which statins provide anti-atherosclerotic benefit. On the other hand, multiple studies link selenium deficiency with an increased risk for cancer and CV disease. Co-Q + selenium supplementation has been shown to improve health and lower disease/mortality in seniors. Thus, I measure selenium levels in my own patients and supplement as needed.
Supplement sourcing is important. Some are better than others. I recommend Vinco RYRE and Douglas Labs berberine. We are currently using Bergamot BDF from Ortho Molecular, but I am open to suggestion here. As a general rule, it is best to obtain supplements from nationally recognized firms who participate in MD/DO education, such as Metagenics and Designs for Health. Low cost supplements from the drug store may be low in quality as well. That’s all I have to say. You now know what I know about HMG Co-A Reductase inhibition. We reviewed a lot of biochemistry, but the more you now, the better will be the decisions that you make regarding how to optimize your own health. Other entries on the heatfixer website and our UTube presentations provide more detail regarding the concepts discussed above.
James C. Roberts MD FACC FAARFM
9/20/19