 12/23/23
12/23/23
VSEL Activation (Focus on Heart Failure)
Dr. Roberts underwent Anti-Aging VSEL
Activation in late 10/22 and every six months since then.
Through 12/20/25, 177 individuals have received a total of
303 VSEL Activations in our office.
40 with advanced pump dysfunction and/or heart failure, have received a total of
124 sessions.
VSEL Activation is discussed below, followed by CV case studies and my analysis.
Our VSEL (very small embryonic-like stem cells) Activation Program triggers
self-repair, such that you can renew yourself. We can provide you with
sample protocols, along with one or more pertinent articles or write-ups.
Basically, we are using physics, to affect biology, to stimulate the body to
rejuvenate itself. VSELs arise at Day 7 post conception, and then migrate to
our primordial organ systems, where they give rise to tissue-specific stem
cells, that can give rise to cells of that tissue and cells of that tissue
alone. The residual VSELs go into growth arrest. They become unresponsive to
growth hormone and insulin, and an inhibitor is placed on their activation
site. They do not proliferate or differentiate, and, thus, remain pluripotent
(able to generate any cell of the human body, but not placenta or a new human).
VSELs concentrate in the bone marrow, but they are present in the circulation,
in a dormant state. In a calamity (tiger bite), the damaged tissue releases
distress and homing signals that activate peripheral VSELs, and pull resident
VSELs out of the bone marrow, and into the circulation, where they begin to
proliferate and release tissue-healing growth factors. VSELs will be pulled
into the site of injury. The chemical characteristics of the damaged tissues,
which pulled in the VSELs, promotes VSEL differentiation into a stem cell
specific to that specific tissue. The now-resonate, activated VSELs release
growth factors and generate daughter cells, contributing to healing of the
damaged region. VSELs also play some role in health maintenance, in that 1% of
our heart cells turn over every year, either from their pool of tissue-committed
cardiac stem cells (which arose from VSELs on Day 7) or by VSELs pulled in by
low-level tissue strain. In a heart attack, VSELs activate and hone into the
heart, where they participate in cardiac repair. As heart attack was not
anticipated by our creator or evolution, heart attack repair is far less
efficient than would be repair of a soft tissue injury, but it does occur. In
animal models, the injection of large volumes of VSELs, soon after experimental
heart attack, leads to prominent cardiac recovery. Thus, qualitatively, we know
that VSELs will promote rejuvenation of the heart and likely any other organ
system (because that is their job).
Inactive VSELs are present in our blood. We withdraw 60 cc of blood, centrifuge it, discard the red cells and white cells, and are left with platelet-rich plasma (PRP). PRP (which contains platelet-derived growth factors, along with inactivated VSELs) has a long history of use in human musculoskeletal medicine. We then apply a specifically-refracted laser beam, which provides a frequency that breaks the bond between the VSEL inhibitor and the VSEL Activation site, “tricking” the VSELs into emergency activation (you can demonstrate this in tissue culture). We do not culture the VSELs, but rather rapidly reinfuse them, and over the next 25 minutes, they will bind to adhesion molecules elaborated by the vessel wall, enter that tissue, and then differentiate into tissue-committed stem cells, and influence regeneration of that region.
We feel (but have not yet proven) that the Modified Laser will also affect the way we read our DNA, promoting elaboration of adhesion molecules. Thus, we “paint” the skin surface over organs of interest, such that they preferentially draw in the administered VSELs. When we treat heart failure, we apply the laser to the heart region (and to the heart region alone, as we want the heart to scarf up all of the VSELs) over 14 minutes. The Anti-Aging Protocol (which I have received three times) (once every six months) directs the VSELs to the brain and endocrine system. I have noticed an energy lift, particularly with respect to running and my recovery from long runs, and that has been the experience of other physicians in our group.
Over our two years, we have provided 232 treatments to 165 individuals, including 32 with advanced pump dysfunction. There have been no complications associated with VSEL Activation (nor would any be expected). The majority of our cardiac patients have experienced clinical benefit, and in most (but not all), their Cardiac Echo findings have improved (over four to eight months). Case studies are provided below.
JH - VSEL Activation in Post-Chemotherapy Dilated Cardiomyopathy
This 74 year old, health aware, health conscious women presented in 9/18 with heart failure, kidney dysfunction (creatinine 1.8 and potassium elevated at 5.8), and evidence of embolic stroke to both cerebral hemispheres. Echo described a dilated cardiomyopathy (DC) picture, with an ejection fraction (EF) of 15-20% (normal is > 55%), mild-to-moderate mitral valve regurgitation (MR), moderate-to-severe tricuspid valve regurgitation (TR), and dyssynchronous left ventricular activation on the basis of left bundle branch block (CLBBB). BNP (B-type natriuretic peptide) a marker of heart failure, was > 5000 (normal is < 370). Pump dysfunction was felt to be due to adriamycin chemotherapy, employed to eradicate breast cancer in 2000. The strokes were embolic; a clot had formed within the dysfunctional heart, broken off, landing in the left hemispheric (leaving JH with a speech deficit), and in the right hemisphere (leaving JH with left sided weakness).
Initial therapy included a diuretic to mobilize retained fluid, along with thoracentesis (needle drainage) to relieve fluid pressure on the lungs. Neuro-endocrine blockade (Entresto and Carvedilol) was begun, along with Digoxin (to stimulate cardiac contractility) and Eliquis anticoagulation (to prevent recurrent embolic stroke). A biventricular pacemaker/defibrillator was placed (to resolve LV dyssynchrony and prohylax against ventricular arrhythmia). JH, her husband, and their personal physician researched cardiomyopathy and JH embarked on a nutritional program that included high dose Co-Enzyme Q10. With these measures signs and symptoms of heart failure improved and kidney function normalized.
In early '19, we rounded out JH's metabolic support program with the addition of Carnitine, Ribose, Taurine, Magnesium, and high dose B vitamin supplementation. Immune modulation with Pentoxifylline was begun, along with Famotidine to block the deleterious effects of Histamine on JH's LV. We met for the first time in 5/19. While echo described persistent pump dysfunction (EF 20-30%) with mild-to-moderate MR, I was impressed by JH's preserved functional status and the absence of physical findings of heart failure.
JH was functionally limited in relation to her presenting embolic strokes. Here JH underwent Relox Stroke Recovery protocol on four occasions (between 5/19 and 12/19), with noticeable but incomplete recovery of speech, balance, and motor function.
In '21 we substituted Ouabain for Digoxin, and JH began a program of periodic therapy with Cheloheart, the Khavinson peptide bioregulator designed to stimulate heart regeneration. JH was thus receiving maximally tolerated neuroendocrine blockade, immune modulation, and every mitochondrial support therapy that we were aware of. Through 2022 JH remained stable, without significant cardiac limitation,
JH underwent Cardiac VSEL activation on 2/20/23 and 4/26/23. NT-proBNP fell from 861 in 1/23 to 488 in 4/23 and to 372 in 7/23 (normal is < 372). Pre-VSEL I estimated JH's EF in the 25-30% range, and in 4/23 and in 9/23 more in the 30-35% bracket. LV chamber measurements are steadily decreasing, a sign of improving pump performance. JH's walking has improved a little further, and probably also her sense of balance. Our impression is that VSEL activation, synergizing with JH's prior program, is mediating recovery of pump function lost to adriamycin chemotherapy in 2020. A third VSEL session was carried out on 9/6/23, with plans to repeat JH's echo assessment in mid-'24.
 12/23/23
12/23/23
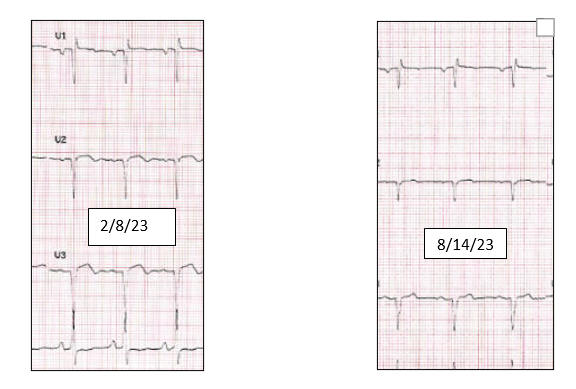
RW - VSEL Activation to address Pump Dysfunction due to Recent Heart Attack
This 72 year old, previously physically active, non-hypertensive, non-diabetic, male non-smoker, with no prior experience with illness, presented in early 12/22 with heart failure on the basis of an extensive anterior wall heart attack, which likely occurred in late 11/22. Diuretic therapy led to a 22 liter diuresis. A culprit 90% mid-LAD (Left Anterior Descending, which serves the front wall of the heart) narrowing was addressed with stent placement. Non-flow restrictive 55% Circumflex (serves the side wall ) and 40% RCA (Right Coronary Artery, which serves the back wall) narrowings were left intact. Neuroendocrine blockade (Carvedilol, Entresto, and Spironolactone) was begun, and diuretic therapy with Bumetanide continued. With these measures signs and symptoms of heart failure attenuated, but RW's functional status did not return to his vigorous baseline. Echo in late 12/23 described an ejection fraction (EF) in the 10-15% range (normal is ≥ 55%). RW was outfitted with a life vest (wearable defibrillator) with plans to implant a permanent defibrillator in two months if his EF did not rise to 30%.
RW was not enthused about defibrillator placement, nor about not feeling his best. RW and I reviewed his situation in early 2/23. Carnitine and and Taurine were added to High dose Co-Enzyme Q10. Neuroendocrine blockade therapy was continued. RW's pre-VSEL echo in 3/23 documented improvement from 12/22, with an EF in the 20-30% range (up from 10-15%) and a decrease in the LV systolic dimension from 5.3 to 4.5 cm (a smaller LV dimension is consistent with recovery of function). Thus some of RW's initial pump dysfunction was due to "stunned myocardium" (to avoid death the heart cells turn off, later to recover function) and some, or course, was due to irreversibly lost heart muscle (or can we do something about this)?.
RW underwent VSEL activation on 3/22/23, and began the corresponding Gematria CV supplements (Systema, Methusalife, Complete Aminos, Heart Gems, Recharge, and Mag Spectrum). Echo study carried out on 4/19/23, at the time of RW's second VSEL activation, showed obvious interval improvement. I graded RW's EF at 30% and felt that regional enlargement in the LAD distribution was less obvious. LV dimensions were further decreased (a good sign), as was the EPSS (a marker of pump dysfunction if above 1.0 cm). Eager to avoid the need for defibrillator placement RW began a program of monthly VSEL activation. Non-pharmaceutical lipid -lowering therapy was initiated, and with this RW's LDL decreased from 196 to 128 mg/dl, and RW completed two months of Cavadex (to pull lipids our of the artery wall and back to the liver). RW's echo studies continue to demonstrate improvement. To my eye, the LAD distribution itself has not come back, but function at the edges of the infarct (heart attack zone) have improved. ST segment elevation (a sign of acute heart attack and later aneurysm formation) has also decreased.
RW's rhythm MD did not feel that a defibrillator was necessary, given this degree of functional recovery. While we have been treating RW's heart, and not using the Anti-Aging VSEL protocol, there certainly seems to be some therapeutic "spillage" of the VSELs to other regions of RW's physiology. RW's overall energy level is better now than it was last summer, his hair is thickening, friends note a healthful change in his appearance, and a certain functional concern in middle-aged men has also resolved.
In animal models, where a large inoculum of VSELs are injected directly into the heart, recovery from heart attack is breath taking. RW is improving, and he improved in a hurry (to avoid the need for defibrillator placement). The heart attack zone has not "filled in" but we need to be a little patient, as we feel that the full effect of a given VSEL activation may not show itself for 6-9 months. Additional VSEL activations are planned, with period echo screening to evaluate pump function, along with ongoing risk factor reduction, Cavadex therapy to promote reverse cholesterol transport, along with a program of EDTA chelation therapy. 12/23/23
|
Date |
Estimated Ejection Fraction |
|
12/28/22 |
10-15% |
|
3/14/23 |
20-30% |
|
4/19/23 |
30% |
|
5/12/23 |
30-35% |
|
7/10/23 |
30-40% |
|
8/14/23 |
35-40% |
SB - VSEL Activation in Heart Failure due to Autoimmune Lung Disease
This 83 year old previously physically active female underwent pulmonary VSEL activation in 3/23 and 10/23, to address heart failure, occurring on the he basis of interstitial lung disease, with a subsequent, progressive improvement in SB's functional status and echo findings.
SB required two-vessel stent placement in '06. We began working together six years later. A comprehensive risk factor reduction program was constructed. Angina has not recurred, a dobutamine stress echo study in '18 returned benign, arrhythmia had not been an issue, and through early '21, SB was swimming laps without difficulty.
Shortness of breath developed in 5/21. The problem then was not cardiac but rather pulmonary (lung disease). SB smoked off-and-on when she was younger, but not beyond her 40's,. The problem was not COPD or asthma. Rather, SB's CT scan revealed diffuse, interstitial lung disease. Pulmonary function study demonstrated a reduced functional lung volume and impaired diffusion of oxygen into the circulation. SB's Antinuclear Antibody (ANA) returned abnormal. This condition is felt to be autoimmune, wherein the immune system mistakes lung tissue as foreign, and then attacks the lung tissue, compromising airway function.
The standard therapy in interstitial lung disease is immune system suppression (corticosteroids and chemotherapeutic drugs) and supplemental oxygen as needed. High dose prednisone (20 mg/day), was begun, leading to fluid retention and a 15 pound weight gain. Echo study in 11/21 demonstrated a pattern of right heart strain. When oxygen exchange is compromised, the pulmonary arteries, which transport blood from the right heart to the lungs, begin to constrict, raising the BP within the right heart (termed pulmonary hypertension); the result is right heart overwork and eventual failure. SB's pulmonary artery (PA) systolic pressure was 47 mmHg (normal is < 25), both the right ventricle and right atria were enlarged, and moderate tricuspid valve insufficiency had developed. BNP (a lab marker of heart failure), was elevated at 223 (normal is < 100). Diuretic therapy (Furosemide 40 mg/day) was added.
I saw SB in 1/22, and found her to be in atrial fibrillation with an elevated ventricular response. Eliquis anticoagulation was initiated and we constructed a rate control program (Carvedilol, Digoxin, and Ouabain) which decreased SB's HR into the normal range. As the problem was lung disease, which was not responding to treatment, as opposed to a reversible heart condition, I felt that any attempt to return SB to a normal heart rhythm would likely cause more harm than good. Losartan (angiotensin receptor blocker) was added for BP and heart failure control. Prednisone had been tapered down to 15 mg/day.
Azathioprine (a chemotherapeutic immune suppressant) was begun in 3/22, allowing a reduction in prednisone to 10 mg/day, but this agent led to liver dysfunction. SB's pulmonary group recommended mycophenolate (CellCept), an agent used to prevent kidney transplant rejection, but SB's insurer balked. Thus prednisone was continued. SB's pro-BNP (upper limit of normal is 624) increased to 1,563.
Our echo study in 7/22 demonstrated persistent right heart dysfunction (PA systolic pressure now 50 mmHg), and new left ventricular dysfunction (ejection fraction 40%) which I attributed to the effects of atrial fib and impaired oxygenation, along with mild-to-moderate mitral regurgitation (consequent to the LV dysfunction).
By 1/23, SB's echo picture had worsened. I estimated her LV ejection fraction at 35-40%. Evidence of right ventricular pressure overload was seen, with a PA systole still elevated at 46 mmHg. Her pulmonary physician had no new ideas. By this time I was feeling the positive effects of my first anti-aging VSEL activation in 10/22. We thus discussed this approach and I asked SB to looked through our literature. I pointed out that VSEL activation does not address autoimmunity per se, but that it might, to some degree, restore some of SB's lost lung capacity. We had no other ideas so why not give VSEL activation a try?
VSEL activation was carried out on 3/17/23. While heart failure was present, the underlying problem was impaired oxygenation, due to autoimmune lung disease, and thus we focused on the lungs. Here, SB inhaled nebulized, activated VSELs, as we directed the infused activated VSELs to the lungs. Supplementation designed to assist in uptake and differentiation of the VSELs into pulmonary in situ stem cells was added (Systema, Methusalife, and Complete Aminos). Endothelial function had faltered (SB's EndoPAT score had dropped from 2.3 to 0.5), so we added Nitroxx (arginine and co-factors designed to increase nitric oxide generation). Pentoxifylline, a gentle immune modulator, of value in heart failure regardless of causation, was added.
Two months post-VSEL activation, SB was feeling a little better. She had stopped furosemide and mild edema was present, so as needed furosemide was resumed. Prednisone remained on board, at a slowly decreasing dose. SB's echo demonstrated a normalization of LV function (EF now 50-55%, mitral regurgitation was less prominent, and SB's LV chamber measurements had decreased from 5.6/3.2 in 1/23 to 4.4/2.8.
The protocol was repeated on 10/2/23. Why not? The more VSELs directed to the lungs, to release growth factors and to differentiated into pulmonary stem cells, the better. We then added in Oxylorem, a growth factor rich supplement derived from seven-day old chicken embryos, which our patients with lung problems have responded well to. VSELs bear receptors for growth factors, and thus a synergy between VSEL activation and Oxylorem is a reasonable expectation.
As of mid-12/23, SB's functional status, while still limited, has continued to improve. Prednisone is now down to 5 mg/day, SB no longer requires her albuterol rescue inhaler, and furosemide is needed less frequently. LV function, as assessed by echo, remains unimpaired. RV function is now back to normal, and echo findings of RV pressure overload and an elevated right heart filling pressure are no longer appreciated. SB remains in atrial fib, now with a HR in the 80s. Prednisone is down to 5 mg/day.
SB bears an autoimmune pulmonary condition that was not responding well to maximally tolerated pharmaceutical intervention. We thus took a multimodal integrative approach and SB is feeling better. SB's current program will be continued and we can carry our VSEL activation #3 as SB's discretion.
 12/20/23
12/20/23
CP - VSEL Activation in Recurrent Atrial Arrhythmia
We might have gotten lucky here, but CP, plagued by recurrent atrial arrhythmia since '16, converted from atrial flutter to normal sinus rhythm (NSR) several days after undergoing cardiac VSEL activation in early 11/23.
11/1/23 11/15/23
This 65 year old, incredibly health conscious, medically proactive, non-hypertensive, non-diabetic, male non-smoker with genomic hyperlipidemia and overactive iron absorption, feels great, able to exercise ad lib, when in sinus rhythm, but when atrial arrhythmia recurs, CP feels poorly, with fatigue and shortness of breath, that progresses to pump dysfunction.
Palpitations first surfaced in 1/16. In 3/16 CP required hospitalization for atrial flutter. Echo described diffuse hypokinesis (a generalized weakness in left ventricular pumping function) with an ejection fraction of 40-45% (many individuals tolerate atrial fib/flutter well, with minimal symptoms and without a drop in ejection fraction (EF), while others, like CP, medically fall apart). A chemical stress study did not reveal evidence of coronary insufficiency. Cardioversion was carried out, CP returned to normal sinus rhythm (NSR), and by 5/16 CP's echo picture had normalized.
Between '19 and the present, this pattern has recurred on multiple occasions. CP has consulted with multiple physicians, and no cause of arrhythmia was uncovered. CP is not hypertensive, diabetic, or hyperthyroid; a sleep study returned normal. Stress studies have all returned negative and when in NSR, CP's echo studies are now revealing only for mild left atrial enlargement, the result of recurrent atrial arrhythmia. CP underwent atrial fib ablation in 11/19, and fib/flutter (the left atrium was altered to address the fib and the right atrium in an attempt to resolve the flutter) ablation in 6/20. The anti-arrhythmic drugs sotalol and tikosyn were tried, along with diltiazem, metoprolol, and ouabain for rate control.
CP researched his situation extensively (I am blessed to have patients like CP). He read Reverse Heart Disease Now. CP takes great care of himself, and follows a comprehensive nutritional program. Genomic iron over absorption was identified (baseline ferritin 432) and rectified with periodic blood donation. Amalgam fillings had been removed, but biological dental evaluation demonstrated that two of CP's root canals were infected, and that one contained residual mercury amalgam. This situation was addressed. Challenge testing demonstrated lead and residual mercury burdens, which CP addressed with oral DMSA and IV EDTA. CP makes good use of sauna therapy to remove fat-soluble organic toxins. A genomic predisposition to impaired methylation was addressed, and CP's homocysteine values remain in the reference range. Genomic hyperlipidemia is present, with an LDL of 212 in 10/19, falling to 150 in 9/23, but CP's carotid intima-media thickness (IMT) is well below average for age, and only mild carotid bulb plaque was identified in 6/14 and in 11/23.
Everyone (CP and the multiple practitioners with whom he has consulted) is doing all they can, but arrhythmia remains recurrent and highly symptomatic. Amiodarone, our most-powerful atrial fib drug (which can cause lung, liver, and thyroid dysfunction) was begun in 6/23 and discontinued in 9/23. CP's electrophyisologist thoughtfully mapped out the options available to CP, with their associated risks and anticipated benefits, and basically recommended that CP give up on rhythm control (keeping CP in NSR) and proceed instead to AV nodal ablation (using a catheter-based technology to destroy electrical communicating between the fibrillating atria and the ventricles), with pacemaker placement to control the ventricular rate. CP would loose his atrial kick (the atria prime the left ventricle, augmenting pump function), but HR control will be achieved. Stated otherwise, CP would remain in atrial fib/flutter, but his ventricular response would be controlled by the implanted pacemaker. Anticoagulation would still be necessary but rate control and anti-arrhythmic meds (which CP does not tolerate well), would no longer be needed. Given all that CP had been through, without success, this approach made sense to me as well.
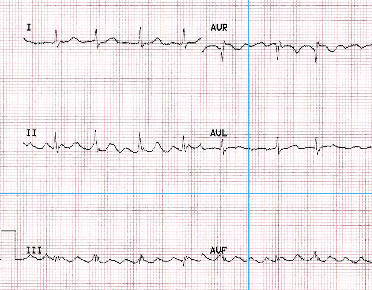
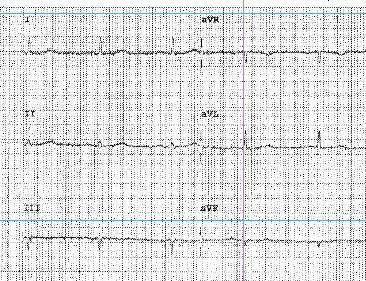
CP was aware of our VSEL program, and the plan was for CP (and Mrs. CP), to come to Toledo for anti-aging VSEL activation in 11/23. At that time CP was in atrial flutter with a controlled (on diltiazem, a calcium channel blocker) HR of 94 (see rhythm strip above). His echo demonstrated mild LV enlargement, and biatrial enlargement. Endothelial function was impaired (EndoPAT score of 1.3), all the sequela of atrial arrhythmia.
My plan was not to carry out cardiac VSEL activation. I couldn't seen how a regenerative approach (our theory is that activated VSELs release growth factors and differentiate into organ-specific stem cells, leading to tissue repair and regeneration) could turn this situation around. I also had a theoretical concern that VSEL activation could "heal" the atrial conduction impairments created by the fib/flutter ablation procedures "undoing" their benefit. CP countered that the ablation procedures had not worked, and that as AV nodal ablation and pacemaker placement were planned, there really was no down side here.
Thus we carried out cardiac as opposed to anti-aging VSEL activation. Three days later, CP called in to tell us that he had converted to NSR, felt great, and that his HR was now in the 40s-50s. We thus decreased CP's diltiazem dose and obtained an EKG (shown above) demonstrating NSR at 58.
How did this occur? What was the mechanism? We feel that activated VSELs, sequestering in a specific organ (in this case the heart) differentiate into tissue specific stem cells which in turn generate daughter cells, renewing the organ involved, and that this process plays out over months (if it takes nine months to generate a new human, tissue repair/rejuvenation post-VSEL activation should follow a similar time frame). We also feel that activated VSELs release growth factors (which bind to cell receptors, more or less instantly affecting their physiology). These growth factors provide anti-inflammatory as opposed to pro-inflammatory effects, and we know that inflammation plays a role in atrial fib (why colchicine, an anti-inflammatory drug that protects against plaque activation, has recently been shown to be of value in the setting of atrial arrhythmia). Thus is CP's case, my hypothesis is that anti-inflammatory growth factors released by activated VSELs resolved atrial inflammation, shutting down atrial arrhythmia. We anticipate that atrial (and ventricular) stem cells, generated via VSEL activation, will strengthen CP's heart and electrophysiology, such that arrhythmia does not recur. We will keep our fingers crossed, and of course CP can undergo further rounds of VSEL activation. I am shocked at how well VSEL activation worked for CP. 12/23/23
1/24 addendum - Following a period of stress, CP experienced 36 hours of arrhythmia with spontaneous resolution.
MR - VSEL Activation in Lone Atrial Fibrillation
Lone Atrial Fibrillation (A Fib) refers to the presence of this arrhythmia in an individual without structural or metabolic heart disease. Stated otherwise, A Fib for no good reason. This designation certainly applies to MR.
MR became troubled by intermittent A Fib in '18.
IV magnesium and meditation/therapeutic breathing techniques helped. Oral
diltiazem for rate control was poorly tolerated while MR did OK with oral
metoprolol.
We began working together in 12/21. We first looked for an underlying
cause(s). MR takes great care of herself, she is neither hypertensive nor
diabetic; sleep apnea is not present. Thyroid chemistries and indices of
methylation returned normal. Complete Right Bundle Branch Block (CRBBB),
reflecting delayed electrical conduction in the right ventricle, was identified,
but we see this is 5% of the population. An echo in 4/18 descried right
ventricular enlargement, but I did not se this on MR's normal 6:32 stress echo
in 4/18. Endothelial function was found to be intact.
One mercury amalgam filling was present, along with a gold crown, possibly with amalgam underneath. A provocative challenge study demonstrated lead and palladium burdens. Amalgams were removed with oral DMSA chelation coverage and MR then received 10 IV EDTA treatments.
We discussed anti-arrhythmic drug therapy and fib ablation (as had her EP cardiologist), but MR did not wish to take this route. She wanted to find and resolve an underlying causes (as would I), and as to therapy to emphasize naturally occurring or regenerative methodologies.
We tried Ouabain, but this agent led to blurred vision, and an unexpected increase in MR's heart rate, Wenxin Keli (used interchangeably with anti-arrhythmic drugs in China) tea, three cups per day, was well tolerated, and seemed to help. MR began a homeopathic digoxin preparation. We use Colchicine to treat gout and to prevent atherosclerotic plaque activation, as this agent bocks the NLRP3 inflammasome, an inflammation augmentation pathway. The inflammasome may be active in A Fib, so we tried Colchicine, without beneficial effect. Frequency Stimulating Microcurrent (FSM), aiming to inhibit sympathetic and enhance parasympathetic function was tried, and had no effect.
In mid-'22, MR received her fourth Covid vaccination. Soon thereafter MR experienced GI symptoms, a rash, and fib changed from intermittent to persistent. Her echo showed only mitral valve prolapse with mild mitral regurgitation, not an explanation for atrial fib. I was our of ideas. MR did not want to undergo Fib ablation, but in persistent fib she didn't feel well.
MR underwent cardiac VSEL activation on 12/12/22. We included an extra 2 minutes to each vagus nerve and to the brainstem (rhythm control centers). The standard post-VSEL activation cardiac supplements were added to MR's program.
Two weeks later, MR was still in A Fib, but she was feeling better. Four weeks out, arrhythmia persisted, but MR was feeling much better. Activities that MR had been avoiding, such as carrying a heavy load up two floors of stairs, were now easy for MR to carry out.
How do we explain this? No objective change occurred in MR's cardiac picture, but her effort capacity had certainly improved. My interpretation is that VSEL activation improved energy generation within MR's cardiac cells; thus her improved functional status. As MR was improving early, as opposed to months post-VSEL activation, I also felt the effect was mediated by growth factors elaborated by the activated VSELs, favorably affecting the function of MR's pre-existent cardiac cells. A less likely explanation was new cell generation (which should take months), from "new" cardiac stem cells, themselves derived from the activated VSEL pool.
A second VSEL activation was carried out on 3/10/23, and a third on 7/12/23, this time a hybrid between the heart, brain and endocrine systems.
Through 11/23 MR feels well, but she is still in A Fib. A colleague is evaluating MR for post-Covid long haul syndrome, looking for persistent inflammation (and if present a means of suppressing it).
I learned about VSEL activation from a patient (everything I do that works I learned from a patient), underwent VSEL activation myself, and now have treated 130 patients. Another patient, with recent bypass surgery, medication sensitivity, difficult to control diabetes and hypertension, and steroid dependent autoimmune disease received IV exosome therapy, with fantastic results. Exosomes are the "therapeutic cargo" of umbilical cord stem cells. I received a low dose, and noticed an up tick in my running and recovery from running (above and beyond that afforded by two rounds of anti-aging VSEL activation). Exosomes provide growth factors, and they also provide an anti-inflammatory biochemical milieu. Thus MR received 5 cc of exosome in early 12/23, and we will will assess her response in early '24. 12/23/23
JW - VSEL Activation in Cardiomyopathy complicated by Parkinson's Disease
In early '17, JW, a previously physically active,
non-hypertensive, non-diabetic, non-smoker, with medically addressed
hypothyroidism and Parkinson's Disease, became troubled by ankle edema and
progressive shortness of breath with effort. Echo demonstrated left ventricular
(LV) enlargement, a generalized reduction in pump function, with an ejection
fraction (EF) of 20-25%, moderately-severe mitral regurgitation, and evidence of
pulmonary hypertension. JW's pro-BNP was markedly increased at 1,982
(normal range is up to 300).
Standard neuroendocrine blockade was poorly tolerated. All but the lowest dose
of Carvedilol (3.1 mg) lead to symptomatic hypotension; vasodilator therapy was
out of the question. All JW could tolerate was Sprironolactone 25 mg/day,
Pentoxifylline 400 mg/day, and Famotidine 20 mg/day, along with Furosemide as
needed for edema control and night time oxygen support.
We did add in as much mitochondrial support as JW could tolerate (at various times, and as JW could tolerate, GI-wise, Co-Q, Carnitine, Taurine, Arginine, NMN, Glutathione, and Resveratrol). We tried the European compounded immune modulator designed to blunt auto-immune attack against the heart (SAM-CV) as well as the Russian Khavinson peptide bioregulator designed to enhance cardiac protein generation. We mixed and matched these therapies, trying to find a combination that JW could tolerate.
This program worked, to a degree. By 12/17, JW's EF was up to 40-45%, mitral regurgitation was then mild-to-moderate, and pro-BNP was down to 212. In 1/23, JW's EF was 30-40%, mitral regurgitaon was only mild, and JW's standard BNP (the range here is < 100) looked great at 14.
This was a good response to an Integrative Cardiology program. JW remained fatigued, but between '17 and early '23, JW and her husband were able to travel to Iceland, the Arctic Circle, Europe, Cuba, Japan, and Greenland (could they be CIA?). JW handled this travel well.
JW underwent cardiac VSEL activation in early 3/23. Soon thereafter JW and her husband took a cruise, with stops at several ports in the Mediterranean, which involved a lot of walking. Her 5/23 echo, just three months out from VSEL activation, demonstrated a slight improvement in pump function (EF 35-45%), and and decrease in LV chamber dimensions (5.8/4.4 to 5.2/3.2 cm.).
I wanted to carry out a second cardiac treatment, but JW opted instead to receive a hybrid anti-aging/Parkinson's protocol (here we attempt to direct the activated VSELs to the substantia nigra, the motion control center, as well as to the brain in general) in late 5/23.
JW and her husband enjoyed a visit to California
(where he received training in the VSEL activation technique) in the fall,
followed by a Caribbean cruise in 11/23.
No signs of heart failure were identified when I saw JW in mid 12'23. She has
reduced her Parkinson's meds by 50% and overall feels better. A follow-up echo is
planned.
My recommendation is that JW receive VSEL
activation once a month, alternating between the cardiac and Parkinson's
protocol (why not - if this is working, why not throw waves of activated VSELS
at the problem?), with periodic echo monitoring, a program that can all be
fine-tuned in relation to how JW responds.
 12/22/23
12/22/23
JM - VSEL Activation in Cardiomyopathy following Bypass Surgery, Mitral Valve Replacement, and Biventricular Pacemaker Placement
This 74 year old, previously physically active, non-diabetic, non-hypertensive, non-smoker with medically controlled hyperlipidemia presented in 4/22 with progressive shortness of breath with effort, advanced pump dysfunction (ejection fraction 10-15%), moderately severe mitral regurgitation (MR), and moderate (70% LAD and 80% RCA) two-vessel coronary disease.
What was the culprit? Was JB troubled by a primary cardiomyopathy, with secondary mitral regurgitaon, with coronary disease as an incidental finding, or with MR the culprit, with consequent pump dysfunction? Or, could the the coronary disease be flow restrictive, leading to ischemic (and thus reversible) pump dysfunction, with secondary MR?
Great question, and the answer was not clear (often it is not), and thus a comprehensive surgical repair was carried out. Bypass grafts were placed to the LAD and RCA and the mitral valve was replaced.
CHF did not resolve. JM returned with persistent symptoms, and a slight rise in pro-BNP to 1,146 (» 1,000 pre-op). Comprehensive neuroendocrine blockade was applied (Entresto, Spironolactone, Metoprolol, and Jardiance), but JM remained symptomatic, with a further rise in pro-BNP to 5,673 in 8/22. CLBBB (complete left bundle branch block) had developed, placing JM's LV at a mechanical disadvantage (with one wall activating a split second before the opposite wall).
JM and I began working together in 8/22. Neuroendocrine blockade was continued, and a mitochondrial support program (Co-Q, Carnitine, Taurine, Magnesium, and Ribose) was added. While coronary insufficiency was not JM's current problem, recurrent disease is a future concern, and thus we added Berberine to complement ongoing statin therapy, hyperhomocysteinemia and hypothyroid physiology were addressed, and Lysine and Proline were added to address a genomic elevation in Lp(a).
JM continued to struggle, with a pro-BNP of 15,272 in 8/22. Echo study in 10/22 revealed persistent pump dysfunction, with an EF still in the 15-20% range. Side-effects of Jardiance led to its discontinuation.
Biventricular pacemaker placement made sense, hoping to improve the mechanical efficiency of JM's left ventricle. This procedure was carried out in the fall of '22, but two months later, in 12/22, JM's pro-BNP was up further, to 15,272. Pentoxifylline (immune modulator helpful in CHF of any cause) and Famotidine (to block the deleterious effects of histamine on the failing heart) were added, and adjustments were made in JM's neuroendocrine blockade and diuretic program. By 2/23, pro-BNP had decreased to 4,707.
By then our cardiac VSEL activation program was up and running. JM was treated on 5/31/23. Since then, we have observed a slow but steady decrease in JM's pro-BNP values (as charted below), with concomitant incremental improvement in her echo findings (ejection fraction is rising, LV chamber dimensions are falling, and TR velocity, a marker of pulmonary hypertension, is lower).
A single VSEL activation has made a difference - a huge difference!. We applied this therapy following cardiac surgery, pacemaker implantation, and a full complement of pharmaceutical and nutritional intervention (all we had to offer). Additional VSEL activation can be carried out at JM's discretion, and we will continue to monitor JM's echo status and pro-BNP levels. 12/22/23
RE - VSEL Activation in Ischemic Cardiomyopathy complicated by Parkinson's Disease
This 81 year old male with compensated heart failure on the basis of ischemic pump dysfunction and atrial fib, underwent cardiac VSEL activation on 5/5/23, with improved echo findings in 8/23. VSEL activation aiming to ameliorate Parkinson's symptoms was carried out on 10/3/23.
RE's initial evaluation in '06 demonstrated moderate aortic insufficiency, not accompanied by LV enlargement, mild kidney dysfunction (creatinine 1.5-1.6), medically controlled hypertension, an elevated Lp(a), and a significant lead burden. A 11:00 stress perfusion study returned negative. EDTA chelation therapy was begun and with this BP control improved as did RE's kidney chemistries. LV enlargement developed in '07 and '08, but pump function remained intact, such that elective valve surgery was not felt to be needed - this was what we going to be watching for.
Our approach changed in mid '11, when new onset chest discomfort led to angiography. Multivessel coronary disease was identified, leading to five vessel bypass and aortic valve replacement.
RE recovered well, and stress echo studies in 9/11 and 11/14 returned benign; prosthetic aortic valve function looked good, and creatinine values were in the 1.2-1.4 range.
In '18 atrial fib developed. Pump function was intact and anticoagulation was added to RE's program.
Shortness of breath, complicating an upper respiratory syndrome, developed in 4/19. Chest X-ray described bilateral pleural effusion. Pro-BNP was increased at 2,444, but RE's echo looked good. Symptoms improved with diuretic therapy. The cause of this setback was felt to be the combined effects of hypertension, kidney dysfunction, and atrial arrhythmia, aggravated by pulmonary infection.
We may have been wrong. Echo study in 9/19 revealed inferior wall hypokinesis (impaired function of the back wall of RE's left ventricle). A chemical perfusion study documented a fixed perfusion abnormality within the inferior wall. RE had sustained a painless heart attack, likely involving the grafts to his right coronary artery. As additional ischemia was not identified (stated otherwise, other regions were not felt to be of risk), and as RE was then feeling better, repeat angiography was not felt to be appropriate.
We did intensify neuroendocrine blockade (Carvedilol, a beta-blocker, Telmisartan, an angiotensin receptor blocker, and Jardiance which promotes fluid mobilization by the kidneys) and a comprehensive nutritional support program was continued. RE underwent several rounds of Cheloheart (Khavinson peptide bioregualtor designed to stimulate generation of cardiac proteins).
RE experienced Covid in late '21, and with this pro-BNP rose from 1,733 to 3,230, and later to 4,713,
Echo in 7/22 revealed an ejection fraction in the 40-45% range, while RE's 5/23 study demonstrated an EF of 35-45%, now with moderate mitral regurgitaon. Creatinine was stable at 1.5.
All of our approaches within the paradigm of Integrative Cardiology were in place, but RE was slipping (aging doesn't help us here).
Cardiac VSEL activation was carried out on 5/5/23. Repeat echo three months later demonstrated a slightly improved EF (40-50%), a decrease in LV dimensions (6.3/4.5 to 4.9/3.4) and pro-BNP had dropped from 4,713 to 4,065.
I proposed repeating the cardiac VSEL procedure, but at this point (summer '23) RE was limited more by Parkinson's than cardiac symptomology, and thus the VSEL Parkinson's protocol was carried our in 10/14. I will be seeing RE in early 1/24, at which point his treatment regimen will be re-evaluated. 12/23/23
TC - VSEL Activation in Dilated Cardiomyopathy with Persistent Sinusitis
TC bears advanced, but clinically compensated, non-coronary pump dysfunction. Chronic sinusitis/asthmatic symptoms are more troublesome. Regenerative measures have recently been applied and we are pleased that both of these conditions are improving.
TC was troubled, in his 20'3 and 30's, by triad asthma (aspirin intolerance, nasal polyps, and asthma). Multiple practioners prescribed multiple treatments, but the only appraoch taht controlled TC's upper airway symptoms was high dose (10 mg/day) prednisone, initially intermittent, and then continuous.
Cardiac trouble surfaced in '16. Late that year TC was hospitalized for heart failure. Atrial flutter with a rapid ventricular response was whipping his left ventricle (LV). Echo described an ejection fraction (EF) of only 5%, with associated moderate mitral regurgitaon. Angiography demonstrated only minimal plaque. Anticoagulation, rate control meds, and neuroendocrine blockade were applied, but tolerated poorly.
When I met TC in 1/17, his rhythm was A Fib with a HR in the low 100s. His EF had improved to around 20%. Fib ablation was offered, but TC did not wish to take this route. A cardiac nutritional support program was constricted and to this we added digoxin, and later diltiazem, and shortly thereafter TC 's rhythm reverted back to sinus (NSR). In NSR TC's EF had improved into the 25-30% range, and mitral regurgitation had resolved.
A Fib recurred in 3/18, but then was better tolerated. TC's EF remained in the 30-35% range. We treated TC with SAM-AL, the peptide immune modulator designed to blunt allergic phenomena, and with this his sinus symptoms improved. TC then transitioned to SAM-CV, the modulator designed to blunt auto-immune attack against the heart, and this helped. We tried to convert TC back to NSR with the anti-arrhythmic drug Sotalol but this agent was poorly tolerated..
TC remained clinically compensated, with an EF in the 25-30% range, between 4/19 and 8/22, but in 7/23, we noted a slip in pump function, with an EF of 20-30% and an increase in LV dimensions..
Oxylorem, a growth factor preparation derived from 7-day old chicken embryos, worked well with TC's sinus/asthmatic symptoms. VSELs have receptors for growth factors and thus we anticipate that this supplement will synergize with VSEL activation. Oxylorem focuses on the lungs, bone marrow, and energy production. Recall, a similar preparation, works a the level of the nervous system, while Relivium targets the GI tract).
TC underwent cardiac VSEL activation on 7/19/23. Six weeks out, TC was feeling better, with some days that he describes as "amazing" and some that are "average". Four months out, TC continues to slowly improve. His sense of smell has returned. Echo demonstrates improved pump function, and a decrease in chamber dimensions.
Our plan is to repeat cardiac VSEL activation in early '24, with a follow-up echo four months later. 12/23/23
KM - VSEL Activation to Inadvertently Compensate Chronic Aortic Insufficiency
In the setting of chronic mitral (please see JB's case study below) or aortic valve insufficiency, the left ventricle is exposed to chronic volume overload. It must pump out its normal stroke volume, to meet the body's needs, but also must propel forward the "back flow" regurgitant volume. The left ventricle (LV) is thus doing its work twice, To accommodate this volume overload pathophysiology, the LV dilates. Thus in chronic aortic insufficiency (AI) the LV diastolic dimension is typically » 6 cm (normal is < 5.6). As long as systolic function, the heart's "squeezing" capacity, remains intact, the LV systolic dimension remains normal, also with a normal to mildly increased ejection fraction. AI and MR are typically well compensated for years, but eventually, if the regurgitant volume is excessive, cardiac contractility begins to wane, and we see a progressive increase in chamber dimensions (particularly the systolic dimension), heralding the onset of heart failure signs and symptoms and the need to repair/replace the faulty valve. Drug therapy in MR and AI really doesn't work, as the problem is mechanical as opposed to medical. Thus our approach involves yearly echo studies (twice a year is we see a change) to guide decision making as to whether observation or referral for valve repair/replacement is appropriate.
KM has a long cardiac history (RCA stent placement in 4/01), and we've been working together since 9/08. KM's cardiac status is stable, and thus KM underwent anti-aging (nervous system and endocrine systems), and not cardiac VSEL activation on 2/10/23, but his 11/23 echo demonstrated a decrease in LV chamber dimensions.
RCA stent placement was carried out in 4/01. An abnormal stress study lead to angiography in 11/02, revealing a new 70% LAD narrowing. The RCA stent was patent and thus single vessel bypass (LIMA graft to the LAD) was carried out. CT angiography in '08 described RCA restenosis and a distal 50% LAD narrowing, but direct angiography revealed only a 50% RCA narrowing, atresia of the LIMA graft, and a now only 50% LAD narrowing. Our impression is that atherosclerosis had regresses within the LAD, and thus flow was directed through the native LAD and not through the LIMA graft, and thus it had shut down. In any event, these were favorable findings.
Angina recurred in '13. Angiography revealed a stable 50% LAD narrowing, a small but still patent LIMA graft (it actually looked better), and now the RCA stent had a 95+% restenotic (scar tissue, not atherosclerotic plaque) narrowing. Our approach here involved EECP followed by a program of regular exercise (KM is a runner) and with this KM's functional status returned to baseline.
Since '13, angina has been non-problematic. We continue to work on risk factor reduction. Palpitations on the basis of PVCs trouble KM intermittently. Kidney dysfunction has been present all along (creatinine 1.4 in '08 and in the 1.5s at present. Vertigo and headache have been problems this year.
In 4/19, echo study demonstrated moderate aortic insufficiency (AI), then without LV chamber enlargement. Non-pronounced LV diastolic enlargement has been seem on KM's yearly follow-up studies, but LV systolic function (ejection fraction and systolic chamber dimension) have remained normal, and thus aortic valve surgery is not felt to be needed, but of course we will be watching for this.
We can prove that the SONG laser activates latent VSELs in our plasma. We cannot prove, but we assume, that the laser can guide the activated VSELs to body sites of our choosing. Having said this, we have seen off-site beneficial changes, suggesting that some of the VSELs are sequestering wherever they wish to land.
We repeated KM's echo in 11/23, seven months our from anti-aging VSEL activation, not to evaluate for a VSEL effect s but to monitor for a worsening of his AI. AI remains. as expected. but we also saw a decrease in LV chamber dimensions, as if we were turning back the clock, rejuvenating KM's heart, such that it could better withstand the volume overload stress imposed on it by chronic AI. In a sense, the loss of LV contractility due to AI or MR is a 'stress aging" phenomena, and we just might have "turned back this clock" in KM. To see if we can build on this theory, in 12/23 KM received 2 ml of exosomes, and we will assess his response in early '24. 12/23/23
JB - VSEL Activation in Cardiomyopathy with Atrial Fib and Mitral Regurgitation
Above, I hypothesized that VSEL activation helped KM's left ventricle (LV) compensate to volume overload on the basis of chronic aortic insufficiency (AI). Will this same compensation occur in the setting of JB's cardiomyopathy with chronic mitral regurgitation (MR)?
In 2/17 JB, a 74 year old, previously physically active, non-diabetic, non-smoker, with medically controlled hypertension and sleep apnea addressed with CPAP experienced chest tightness and shortness of breath that was initially felt to be upper respiratory in nature. JB's evaluation, however, demonstrated atrial fibrillation with a rapid ventricular response, advanced pump dysfunction with an EF in the 20-25% range, an elevated BNP of 829 (upper limit of normal 100), and moderately severe mitral regurgitation (MR). Angiography demonstrated a 90% LAD narrowing. LAD stent placement was carried out but had no effect, arguing that LAD ischemia was not the culprit. At this point it wasn't clear whether non-ischemic pump dysfunction (Dilated Cardiomyopathy) was the primary problem, with secondary MR and A Fib, or rather, that chronic mitral regurgitation was the key issue, with secondary LV failure.
In the later setting, with LV failure due to long-standing MR, valve replacement is not advised, as the LV will not "come back" with correction of the MR. In the former scenario, if LV function improves, secondary MR may also attenuate. Neuroendocrine blockade (Carvedilol, Spironolactone, and Losartan) was initiated. Electrical cardioversion on the anti-arrhythmic agents Tikosyn and Amiodarone was not successful. Carvedilol (a beta-blocker) provided for rate control, and Pradaxa anti-coagulation was begun to prevent atrial clot formation. CPAP wasn't getting the job done, but with a switch to BiPAP JB's AHI (Apnea-Hypopnea Index) normalized. A stress test in 6/17 did not demonstrate recurrent LAD ischemia.
JB and I began working together in 7/17. At that time JB was reasonably well compensated, his BNP had decreased to 185, and while not feeling great, JB was able to carry out necessary activities and negotiate the stairs at work without difficulty. JB's HR was in the 80s. I graded JB's EF in the 25-35% range, and noted moderately severe MR and LV enlargement (LV 6.3 cm. diastolic and 5.0 cm systolic dimension).
JB had two CHF setbacks, both precipitated by infection (viral pneumonia in 2/18 and Covid in 10/21), both times clearing with a transient increase in diuretic therapy.
To standard neuroendocrine blockade (Carvedilol, Losartan, and Spironolactone), we added Jardiance. A comprehensive cardiac nutritional support program was constructed. JB received one year of SAM-CV, the European compounded immune modulator designed to blunt immune attack against the strained heart, and JB completed several rounds of Cheloheart, the Khavinson peptide bioregualtor designed to increase generation of cardiac muscle protein. Ouabain was added and seemed to provide JB a lift.
Thus we had maxed out the therapies that I was aware of. Prior to VSEL activation in 11/22, JB' LV diastolic dimension (LVd) had been trending up, while the systolic dimension (LVs) was stable to improved. 2-3 months post VSEL activation, in 2/23, JB noted a slight improvement in stamina when climbing stairs. His EF was a little better, then in the 35-40% range, and his LV dimensions had decreased from 7.2/4.9 to 6.6/4.7. We thus repeated the procedure on 2/23 and again in late 12/23. Jardiance was stopped in the fall of '23 (insurance co-pay rose ridiculously), and with this pro-BNP (different reference range vs. the standard BNP) rose from 1909 to 2099. His LVs has increased, but remains improved vs. the pre-VSEL baseline. JB remains essentially asymptomatic.
Putting all of this together, I now feel that JB's primary problem was mitral regurgitaon, long-standing, with slowly progressive LV dysfunction, asymptomatic until A Fib developed, to precipitate heart failure (this is what I think and of course I could be wrong). The 90% LAD narrowing was likely clinically silent. With medical therapy, nutritional support, the other novel treatments that we used (compounded immune modulator and Khavinson peptide bioregualtor), we have helped JB's heart compensate for this volume overload stress.
With VSEL activation, we are hopefully "turning back the clock", directing VSELS into JB's heart, with the anticipation that they will differentiate into cardiac stem cells, which in turn will generate functional daughter cardiac cells. JB's improved functional status brings up the question as to whether MV surgery would now be advisable. Risk would be significant, and as JB is now doing so well, our plan will be to continue with our comprehensive non-surgical approach, with periodic echo monitoirng. 12/22/23
Additional case studies will be presented as follow-up data becomes available.
Observations and Analysis
What did we learn over our first year of VSEL activation?
1. VSEL activation is safe. There are no downsides (other than two IV sticks). Nor would a downside be expected, as with VSEL activation we are simply triggering Mother Nature's rejuvenative response to injury, here using physics (refracted laser frequency) to activate latent VSELs in your own plasma, as opposed to a true calamity (our intrinsic trigger for VSEL activation), to initiate cellular repair, repopulate organs with fresh cells (our theory) to improve organ function (at a time and place of our choosing) .
2. Our patients are getting better, as documented above. No one is getting a brand new heart (our patients are not responding as well as did the subjects in the Armenian study), and a few patients didn't feel as if a benefit occurred, but the majority have noted a functional lift and/or an improvement in their non-invasive testing (echo or a change in BNP values), why 16/27 have undergone additional treatments (including some who have undergone Parkinson's or Anti-Aging VSEL activation following their cardiac session, or visa verse). I will point our further that none of our VSEL patients underwent VSEL activation as an initial or mono-therapy. Like EDTA chelation therapy and EECP 25 years ago, our initial approach has been to apply Cardiac VSEL activation only to our patients who were maxed out on our prior best treatment regimens - people who had nothing to lose and something to gain, and gain they have.
3. Cell biology and energy generation improve before anatomy changes (and sometimes anatomy does not change). We would all like to see an improvement in ejection fraction, or other "objective" findings, but this doesn't always occur, and a lack of gross echo change does not mean that patients are not experiencing benefit. MR did not convert to NSR but her functional status certainly improved, indicating that cardiac biology and energy generation did. In our patients with chronic mitral and aortic regurgitation, their dysfunctional valves did not self-repair (nor would we expect this - they are torn), but their ventricular compensation did, as if we biochemically "turned back the clock" with a wave of VSEL support.
4. We need to be patient. If we add in a new anti-hypertensive drug, we check your BP one week later. VSEL activation doesn't work this way. While growth factors elaborated by activated VSELS may provide an early functional benefit (how CP converted from atrial flutter to normal rhythm in 1 week), we do not expect to see anatomic change for 4-6 months (thus instead of obtaining your first post-VSEL echo at two months, we are delaying to four), and perhaps not maximum benefit for 6-9 months (if it takes 9 months for a Human to form up, why should an organ rejuvenation effect due to VSEL activation take less time)?
5. Repetitive treatments provide additive benefits. We feel that any benefit from VSEL activation will be persistent. The "new" cells will last forever (well, as long as the rest of you lasts). Repeat VSEL activation will simply sow another wave of activated VSELs into your organs, amplifying the initial benefit. My plan is to receive Anti-Aging VSEL activation every six months, as a matter of course. Should I sustain an injury (too much running), then I might treat myself monthly until the injury heals.
6. Activated VSELs do not all sequester to the targeted regions. We attempt to direct the activated VSELs to organs of interest, but some are "spilling over". We made no attempt to direct VSELS to KM's heart, but nonetheless his LV chamber dimensions decreased. Patients report benefits outside of the treatment zone - nothing wrong with this!.
7. Predicting efficacy, pre-VSEL activation, is not possible. Logically, the greater one's circulating VSEL pool, the greater will be one's response to VSEL activation. Youth and insulin sensitivity (lean stature and normal blood sugar) correlate with greater plasma VSEL counts (our clinical labs are not able to measure VSEL levels - only research labs). My observation is that younger patients (including me at age 68) demonstrate a brisker response than do older patients (in their late 70s and 80s). Kidney dysfunction leads to bone marrow suppression and declining VSEL counts, but one 80 year old with near end stage renal disease stabilized over the course of one year, while a younger (late 60s) patient worsened despite three rounds of treatment.
8. How can we enhance our response to VSEL activation? VSELS release growth factors, and in turn have receptors for growth factors. There is a literate on growth factor (VEGF, BFGF, an alphabet soup of growth stimulating peptide fragments) therapy in heart failure. Many of our patients are benefiting from growth factor preparations (Recall, Oxylorem, and Relivium) derived from 7-day old chicken embryos, and thus we encourage their use post-VSEL activation. Dr. Ovakaitys, who invented this approach, offers a line of supplements (Gematria) that he feels amplifies the VSEL effect (and he has demonstrated efficacy with his Complete Amino™ and Nitroxx™ preparations in separate clinical trials), so their concomitant use makes sense. I learned about VSEL activation from a patient who Dr. Ovakaitys treated. Another patient benefited from an IV infusion of exosomes, growth factor messengers derived from amniotic fluid mesenchymal stem cells. I received a 2 ml dose and noted a lift (I am up to 18 miles, over 1 1/2 football games, on my treadmill every Sunday). My next VSEL activation will be preceded by a similar exosome infusion. A synergy is expected (the down side here is that I am spending a lot of money on new running shoes)! We will look for (and perhaps stumble upon) additional means of getting the most we can out of VSEL activation, such that we can optimize it's efficacy in patient care.
After all, that is what Integrative Cardiology is all about.
The above are my thoughts, some of which I can substantiate, and some that are my hypothesizes. More to follow as we learn more. James Roberts MD FACC FAARFM 12/26/23