Return to CHC Home Page
Return to Diagnostic Studies
ENDOTHELIAL DYSFUNCTION
Return to Medical Topics Page
The Risk Factor of Risk Factors
Physiologic endothelial function, Nitric Oxide (NO) as opposed to predominant
Superoxide (SO) production within the vascular wall, is a key determinant of
short, intermediate, and long-term cardiovascular health. Oxidative endothelial
dysfunction is the final common pathway through which risk factors lead to
plaque formation, progression, and activation. Endothelial dysfunction reflects
vulnerable biology and increased risk. Peripheral endothelial dysfunction also
reflects metabolic oxidative stress and impaired contractile function of the
heart muscle.
The endothelium refers to the single layer of cells that line our arteries and veins, a mass of tissue the size of the liver. Think of the endothelium as a biochemical factory, the leading edge of the atherosclerotic (and anti-atherosclerotic) process. Mediators (or more precisely the balance of mediators) generated by the endothelium determines blood vessel dilation vs. constriction, platelet stickiness vs. non-stickiness, oxidative stress vs. vascular wall antioxidant function, an uncontrolled vs. a modulated vascular wall inflammatory response, etc. Stated otherwise, control of the endothelium leads to control over the atherosclerotic process.
Flow Mediated Vasodilation is used to measure endothelial function, and together with Carotid IMT to gauge the success or failure of our risk factor reduction efforts. In response to increased blood flow (how exercise and EECP help you) the endothelial cells lining our arteries convert Arginine into nitric oxide. Nitric oxide (NO) in turn rapidly dilates the artery.
For testing purposes, we use non-invasive pulse amplitude tonometry (PAT) to measure blood flow at the level of the fingertip. A BP cuff is inflated above systolic pressure for five minutes, limiting blood flow to the arm. The cuff is then released, blood rushes into the arm, and this increased flow leads to increased nitric oxide generation and blood vessel dilation, to a degree determined by the level of endothelial health that you bear. Accuracy and predictive value of the EndoPAT device correlate well with other invasive and non-invasive means of endothelial testing. EndoPAT is FDA approved and insurance covered (with a few exceptions) for individuals with CV conditions. Testing is convenient, reproducible, and without risk to you.
An EndoPAT score below 1.7 is abnormal, and correlates with endothelial dysfunction as determined by invasive testing; 1.7 to 2.0 is borderline, and a score > 2 reflects intact endothelial tone. We will measure your endothelial status under pristine conditions, early in the day, with an empty stomach, and hopefully in a low stress environment. If we were to repeat your study after a sugar load or high fat meal, when you are stressed, or following exposure to cigarette smoke or automobile exhaust, we would see a decrease in your score. Following stent placement, the “distal vessel” (the coronary artery beyond the point of stent placement) will experience endothelial dysfunction for a period of time (and this would not be reflected in the peripheral EndoPAT measurement). While peripheral EndoPAT testing accurately reflects endothelial tone in a non-obstructed coronary vessel, a normal EndoPAT score can’t definitively exclude impaired NO generation beyond a high-grade blockage (correlating invasive testing is not possible in a severely narrowed vessel). Thus, we will not look at endothelial tone as “normal’ or “abnormal”, but rather on a continuous basis (like BP and lipids). A “higher is better” approached will be utilized in patients with active disease or multiple risk factors.
We’ve carried out your EndoPAT evaluation and determined your score. Now, what can we do to increase your score and thus optimize your level of vascular protection? Plenty, if we understand and support the factors that contribute to endothelial health.
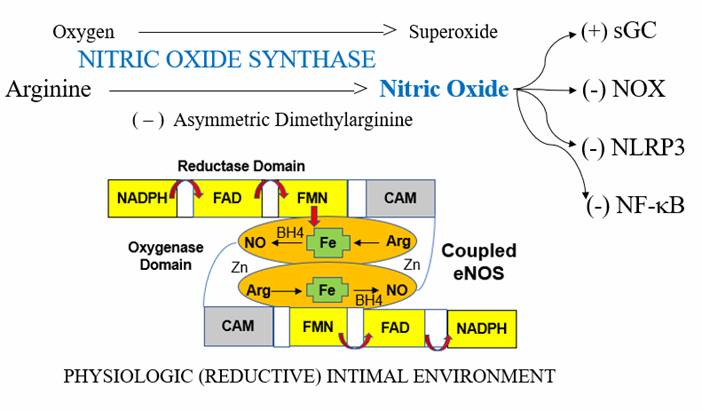
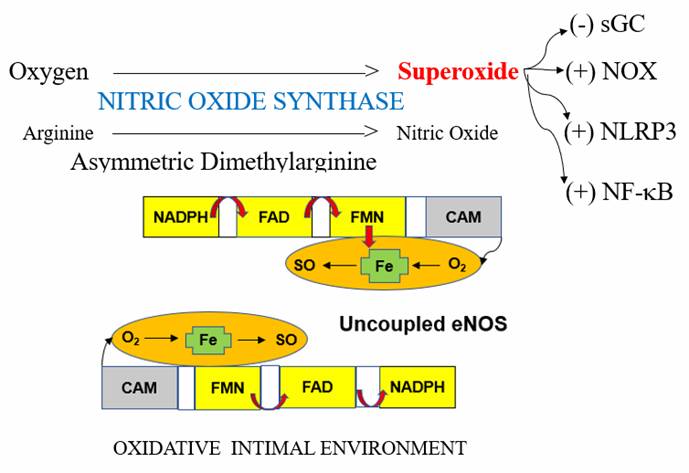
When things are going well, the enzyme Nitric Oxide Synthase (NOS) converts dietary Arginine into Nitric Oxide (NO). It is NO that dilates our vessel, renders platelets non-sticky, and resists plaque formation. NO in turn down regulates (decrease the activity of) pro-oxidant and pro-inflammatory vascular pathways such as NADPH Oxidase (NOX in the diagram) which generates Superoxide (SO), NF-kB (inflammation amplification), and NLRP3 (activates pro-inflammatory cytokines, leading to plaque destabilization). It is NO that takes the “vulnerability” out of vascular biology. From the perspective of preventing and/or stabilizing CV disease, NO is a good thing. We want a lot of it.
In biology, however, too much of a good thing, at the wrong time, can be a problem. Let’s say you got up one morning, left your cave, and got bit by a saber tooth tiger; your wounds bleed and your BP begins to fall. Or maybe you ran out of water during a trip across the desert in search of food, or you developed sepsis when a wound failed to heal. In these conditions, we don’t want NO dilating our blood vessels or inhibiting clot formation. We want the opposite, and here Mother Nature gives us Superoxide (SO), the antagonist to NO. Superoxide is a free radical. It instantly cancels out NO, degrading it into Peroxynitrite (ONOO), a powerful free radical species that in turn converts NOS into a SO as opposed to NO generator. SO (or a lack of NO), in turn activates pro-oxidative and pro-inflammatory pathways.
This process is adaptive in the setting of true infection or injury. Here we call it endothelial activation, not endothelial dysfunction. In these scenarios we want vasoconstriction and enhanced clotting (so we don’t bleed out following the tiger bite) and a heightened immune response (to kill the invading microbes).
It is in our best interest to possess an adaptive endothelium, able to activate, to deal with infection and focal trauma. If you gash your arm, you want endothelial activation in that arm, but not elsewhere. Focal infection should be addressed with focal endothelial SO generation, while elsewhere the endothelium should be converting Arginine into NO and not into SO.
How does Mother Nature throw the switch? What tells NOS to generate SO as opposed to NO? The key determinant is the focal and/or systemic level of oxidative stress. Oxidative stress, SO generation outpacing antioxidant neutralization, the driving force of CV disease, is discussed in detail in the Atherosclerotic Oxidative Stress section of heartfixer.com and in Chapter Three in Personalized and Precision Integrative Cardiovascular Medicine (Walters Kluwer – Edited by my colleague Mark Houston MD). Stated simply (do I actually ever say anything that is simple?), SO excess forces NOS to stop generating NO and to instead make more SO (adaptive in infection and disastrous in the setting of chronic, inappropriate, oxidative stress - the condition of Western Man with risk factors and chronic illness). The intermediate biochemical steps, steps where we can intervene therapeutically, are an excess of ADMA to Arginine, and oxidative degradation of the folate look-alike BH4 (tetrahydrobiopterin). Let’s discuss these steps.
ADMA is short for Asymmetric Dimethylarginine, Arginine with two methyl (CH3) groups attached. When the ratio of ADMA to Arginine is high, NOS stops making NO and starts generating Superoxide. Next question – what factors determine ADMA levels, the ADMA:Arginine ratio, and thus NO vs. Superoxide production?
ADMA ——————————> Inactive
DDAH
( – ) Risk Factors
ADMA is generated at a constant rate and is excreted by the kidneys (kidney disease leads to vascular disease via the mechanism of impaired ADMA excretion). ADMA is degraded by the enzyme DDAH (Dimethylarginine Dimethylaminohydrolase). If we do not want vascular disease, we want DDAH functioning normally, to prevent a buildup of ADMA. All CV risk factors lead to oxidative stress, which in turn inhibits DDAH, leading to a high ADMA:Arginine ratio. NOS then generates SO as opposed to NO, endothelial dysfunction follows, and then CV disease. The long-term risk factors (and the oxidative stress they generate) born by modern man are interpreted by our physiology as threats to the short-term survival of primitive man (think of risk factors as “pseudo-infection” cues), and this leads to the long-term maladaptive process that we call atherosclerosis, initiated and driven by oxidative stress and endothelial dysfunction.
What can we do to lower the ADMA:Arginine ratio and prevent vascular disease? We can resolve our risk factors. If we lower cholesterol, BP, homocysteine, glucose, etc., lose weight, stop smoking, clear toxins, and deal with sleep apnea, oxidative stress will lessen, DDAH will be dis-inhibited, ADMA will fall, and NOS will start cranking out NO as opposed to SO. However, if we cannot (or cannot rapidly) resolve our risk factors, what we can do is to supplement with Arginine, to “rebalance” an elevated ADMA:Arginine ratio. During health, there is plenty of Arginine available. NO production is normal and providing additional Arginine does nothing. Your BP will not fall and you will not begin to bleed; rather nothing will happen. However, if due to risk factors and oxidative stress your high ADMA:Arginine ratio has shut off NO production, supplemental Arginine will rebalance the ratio. You still have a high ADMA level, but if we counter with extra Arginine, the ADMA:Arginine ratio will fall, and it is the ratio, not the absolute levels of ADMA and Arginine that determine the activity of NOS. Thus, Arginine is a universal antidote for endothelial dysfunction. Arginine has been shown to improved endothelial function when it is compromised by risk factors. Via the mechanism of improved endothelial function, Arginine therapy has been demonstrated to improve symptomatic status and/or outcome in all forms of chronic CV disease. Pain improves and treadmill time increases in patients suffering from angina or claudication. Heart failure patients enjoy a better quality of life and effort capacity. Erectile function (if vascular and not neural or due to low testosterone) may improve. Arginine has universal preventive value when risk factors are present. In head to head competition, Arginine is equal to and in some patients superior to statin therapy with respect to improving endothelial tone (the ultimate mechanism through which statins and other pharmaceutical preventive agents work).
NOS, when functioning normally, generating NO as opposed to SO, exists as a dimer, two NOS enzymes bound together, with a key co-factor, tetrahydrobiopterin (BH), in its non-oxidized state (BH4). When SO is generated in excess, at a level outpacing the ability of SOD (Superoxide Dismutase) to degrade in to Hydrogen Peroxide, then it will react with NO to form peroxynitrite (ONOO). ONOO rapidly degrades BH4 to its oxidized or “spent” state, BH2. NOS then “uncouples” into its monomeric form (see diagram above) that converts Arginine into SO.
NO lasts 1/10th to 1 second. We store NO by reacting it with sulfhydryl (SH) bearing molecules, such as cysteine and glutathione. SH bearing molecules are destroyed by free radicals and they are tied up by toxic metals, especially Mercury.
Thus, we wish to bolster our antioxidant defenses, with special emphasis on SH bearing antioxidants (such as N-Acetyl Cysteine) and SO neutralizers (such as Vitamin C, Co-Enzyme Q10, and pomegranate). Bioflavonoids stabilize Vitamin C, explaining how tea consumption, red wine, and cocoa all improve endothelial function.
Methyl-folate squelches peroxynitrite (ONOO). Also, the structure of methyl-folate is similar to that of BH4. Thus, high dose methyl-folate can “stand in” for BH4 and restore lost endothelial tone. Folate/methyl-folate supplementation thus helps to restore lost endothelial tone.
Magnesium is required to generate the energy needed to power NOS. In patients with angina, magnesium supplementation has been shown to improve endothelial function, symptomatic status, and treadmill time. A fluid endothelial cell membrane is needed for Arginine to enter and NO to exit the endothelial cell, and via this mechanism fish oil supplementation improves endothelial function and outcome in CV disease states. Taurine helps with magnesium retention, specifically neutralizes the damaging free radical hypochlorous acid (HOCL), and by these and other mechanisms improves endothelial function.
Nitric oxide also had a powerful immune modulating effect. Our Immune Mechanisms in CV Disease presentation (a three-part UTube presentation available on heartfixer.com) discusses the deleterious effects of chronic inflammation and immune dysregulation. High levels of vascular wall NO will keep vascular inflammation in check (blunts NF-kB translocation). Treatments that improve endothelial function and lower oxidative stress will thus also attenuate inflammation. If you review our IMT (Intima-Media Thickness) presentation, you will see that these metabolic interventions also improve IMT. Inflammation, endothelial dysfunction, IMT, and plaque formation are all different expressions of a common biological flaw – high SO and NO. We can fix this, and in doing so improve your CV and overall health.
While NOS dysregulation is our most important endothelial biochemical problem, up regulation of ACE (Angiotensin Converting Enzyme) is a close second. In the circulation, the product of ACE, Angiotensin II, is a vasoconstrictor, a cause of hypertension and fluid retention. Blockade of ACE has been a main stay of hypertensive management for 40 years. However, the majority of ACE is present within our cells, and within the endothelium, the generation of Angiotensin II leads to SO formation, and with this endothelial dysfunction and immune dysregulation. Blockade of endothelial ACE with a fat-soluble ACE inhibitor
Angiotensin I ———————> Angiotensin II
ANGIOTENSIN CONVERTING ENZYME
(quinapril and ramipril but not lisinopril or enalapril), or an agent that blocks the angiotensin receptor (ARBs – angiotensin receptor blockers) will blunt SO formation, improve endothelial tone, and quiet down an abnormal vascular wall immune response. If your BP is at all elevated, or if you have heart failure, I will emphasize this class of drugs in your treatment (Quinapril has been shown to improve outcome in certain coronary conditions even when BP is normal). The use of these drugs is associated with a high benefit to risk ratio.
Cholesterol enrichment of the endothelial cell membrane compromises endothelial function. High cholesterol ® endothelial dysfunction ® increased endothelial uptake and oxidation of cholesterol ® immune dysregulation ® CV disease. If the cholesterol is oxidized, this progression is accelerated. Low cholesterol is associated with a reduced risk of atherosclerosis. If you have atherosclerosis, lowering cholesterol (and blunting its oxidation) will be beneficial. Statin drugs will lower cholesterol, but that is only part of how they work (please see the HMG Co-A Reductase Inhibition to Lower LDL write-up on heartfixer.com). Statins block the cholesterol biosynthetic pathway at a step that would otherwise activate several pro-inflammatory pathways (conditions that lead to increased cholesterol production also up regulate our biochemical “fight the infection” response). One of these pathways, Rho Kinase, up regulates the production of SO within the artery wall. Statins block Rho Kinase, and when Rho Kinase is up regulated (and SO levels are thus high), statin therapy will improve disordered endothelial function (why statins improve outcome in active CV disease even when cholesterol is normal). Conversely, when Rho Kinase is not up regulated, statin therapy has no effect on oxidative stress and thus endothelial tone. Thus, the relative benefits of statin therapy rise in relation to the degree of inflammation and oxidative stress present. Statin therapy is more valuable to you when plaque is unstable as opposed to when plaque is stable. Statin therapy has some downsides (mediated via reductions in Co-Enzyme Q10, Vitamins D and K2, and steroid hormone generation; downsides that we can measure and rectify). If you just experienced your third heat attack following your second bypass surgery, then statin therapy is right for you. Conversely, the use of statins in younger patients with uncomplicated high cholesterol probably has more long-term down side than benefit. Red Yeast Rice Extract (RYRE) contains several naturally occurring statin compounds, and while less powerful than statins with respect to cholesterol reduction, RYRE will provide qualitatively similar anti-inflammatory and pro-endothelial benefits (we can also use Bergamot, Amla, and Delta-tocotrienols in this fashion). One important note, when the ADMA:Arginine ratio is elevated, statin therapy will not improve endothelial function, while Arginine monotherapy, or Arginine + statin therapy will. Remember, there is no rule that says we have to be drug only or nutritional only doctors and patients. The goal of this practice is to integrate the best of pharmacologic/invasive cardiology with the principles of nutritional/detoxification medicine to obtain the best outcomes for you!
The two most important enzymatic generators of SO are NOX (NADPH Oxidase) and XO (Xanthine Oxidase). Their expression is induced by risk factors, impaired oxygen availability, heart failure, and other sources of SO excess. Drugs that work by down regulating expression of NOS include statins, ACEs and ARBs, Spironolactone, Hydralazine, Colchicine, and the third generation Beta Blockers Carvedilol (Coreg) and Nebivolol (Bystolic). Pentoxifylline down regulates NOX indirectly by blunting inflammation. Nutritional NOX inhibitors include berberine and polyphenols such as pomegranate
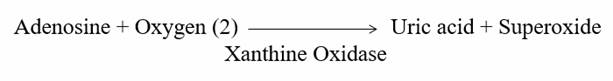
Xanthine Oxidase (XO), the expression of which is upregulated in coronary insufficiency, heart failure, and oxidative stress in general, wastes precious oxygen to generate uric acid and SO. Allopurinol inhibits Xanthine Oxidase (XO), lowers SO generation, protects the endothelium, and preserves oxygen for appropriate energy generation. Allopurinol (discussed in a UTube presentation on heartfixer.com) will predictably improve endothelial function (and clinical outcomes), and we can use Allopurinol for these purposes.
We should note that pulsatile, normotensive arterial flow stimulates NOS, while hypertensive flow stimulate NOX and XO. Thus, the role of regular exercise and BP control.
Taurine and N-Acetyl Cysteine support the generation of Hydrogen Sulfide (HS) which in turn supports NO (you will hear more about HS, NO’s “best biological friend”, in the future). GliSODinÒ provides exogenous SOD, thus assisting in SO neutralization.
Enough biochemistry! Now for a Plan of action. We’ve measured your level of
endothelial function, and determined that endothelial support is appropriate. We
can choose from one or more of the below-listed approaches, repeat your EndoPAT
assessment, and take additional corrective steps as needed. My recommendations
will be tailored to your individual CV status, but a generic approach is given
below:
1. Arginine supplementation – relatively low in cost and essentially risk
free*. Options include:
A. Standard Arginine 4,000 mg (1 & 1/3rd teaspoon) three times a
day. The poor taste can be masked (to some degree) by mixing the Arginine
powder in warm water. Arginine has a short half-life; once-a-day dosing is not
adequate.
B. NOx Synergy (Designs for Health – link on our website) 1 to 2 tsps. twice a
day. One tsp. provides 750 mg Arginine, 750 mg citrulline, 500 mg taurine, 80
mcg methyl-folate, 60 mg magnesium and 125 mg bioflavonoids.
C. ArginCor (Metagenics - link on our website), 1-2 scoops twice a day. Two
scoops provide 3000 mg arginine, 680 mcg methyl-folate, and 2 gm. Of beet root
powder.
D. Hybrid therapy – ½ dose Arginine (lowest cost) mixed with ½ dose NOx Synergy
or ArginCor (higher cost) to mask the taste of pure Arginine powder.
E. Nitroxx (Gematria) 2 three times a day (best away from meals) contains
arginine activated with the SONG Laser (that we use in VSEL Activation).
2. Co-factor support will be a function of your nutritional assessment, ** but
as guidelines:
1. N-Acetyl Cysteine 500 mg daily (+/- Lipoic Acid 300 mg) and Vitamin C 500 mg
twice a day.
2. Magnesium Glycinate (Metagenics) 100 mg, 1-3 twice a day.
3. Folic Acid 1-5 mg/day or preferably methyl-folate 800-5000 mcg/day.
4. Fish Oil 2,000 mg/day. 5. Taurine 500-1000 mg twice a day. 6. Berberine 500
mg twice a day.
7. Life Extensions Endothelial Defense with GliSODinÒ
and Pomegranate twice a day.
3. Pharmacologic NOX and XO inhibition. While we prefer to minimize drug intervention, if your endothelium is on fire, we need to douse the flames, and do so rapidly and here we will exploit the benefits of ACEI/ARBs, Statins (or Red Yeast Rice Extract), Colchicine, Allopurinol, Spironolactone, Pentoxifylline, Hydralazine, Bystolic, or Carvedilol.
4. Hormonal support. Estradiol in women, testosterone in men, and DHEA in both genders supports endothelial function. Conversely, the reduction in endothelial function seen with ageing is in large part due to a loss of hormonal support. Hormone replacement therapy improves endothelial function (this is the key mechanism through which testosterone replacement therapy improves endothelial tone, blunts inflammation, and improves symptomatic status in men with CV disease). There are a number of pros and cons to hormone replacement therapy, but if you chose to receive HRT, we would utilize bioidentical molecules, delivered in a physiologic fashion, with close monitoring of hormone levels and hormone metabolites.
5. Detoxification of pro-oxidant metals and organic pollutants. When I trained atherosclerosis was a disease of old men and much older women. These days we see heart attacks in 50-year olds with normal cholesterol levels. Environmental toxins deplete our nutritional reserves, generate oxidative stress, and damage our endothelium and our DNA. Remove these toxic molecules from your body! I trained in chelation therapy 25 years ago and teach this technique to other physicians and served as an investigator in the NIH Trial to Assess Chelation Therapy. We are ready to help you remove toxic metals and organic pollutants from your body.
6. Pharmaceutical and botanical NO donors are available. The former actually worsen endothelial function and the latter do not improve it.
Sublingual nitroglycerine (NTG) will attenuate angina. One molecule of NTG is converted into one molecule of NO in a process that generates one molecule of superoxide free radical. As superoxide generation is short-lived, endothelial tone is not compromised, and you can take another NTG later in the day and it will still work. Long-acting nitrates (Isosorbide Dinitrate or Mononitrate) release a trickle of NTG, helping with angina control, but also a trickle of superoxide, compromising intrinsic endothelial tone. Thus, you stop making your own NO and angina worsens (termed nitrate tolerance). We would thus increase your long-acting nitrate dose, here again providing only a transient benefit. It has been shown that long-acting nitrates, while helpful in angina control, are associated with a worsened clinical outcome (because they cause endothelial dysfunction)! Fortunately, nitrate induced endothelial dysfunction can be prevented with concomitant nutritional endothelial support (the classic example here is N-acetyl cysteine, which prevents nitrate-induced endothelial dysfunction and augments nitrate efficacy), or with the use of other drug-non-drug endothelial supports.
Beet Root Powder is being marketed to increase NO generation and to improve
endothelial function. Beet Root contains nitrate, which will be converted by
gut microbes back into NO, providing a short-lived burst of NO. There is
nothing wrong with this approach, and in contrast to pharmaceutical nitrate
therapy, the conversion of Beet Root nitrate to NO does not generate
superoxide. However, this approach does not correct underlying endothelial
dysfunction, and thus dysfunctional NOS is still cranking out SO as opposed to
NO. Beet Root Powder is thus an ameliorative, and not a means of normalizing
endothelial tone. The Beet Root people often state that we cannot convert
arginine into NO, and that we must take their preparation. That is not a true
statement! Hundreds of papers demonstrate benefit of arginine in nearly all CV
conditions. They recommend measurement of salivary NO as a measuring stick of
endothelial tone. I compared salivary NO with EndoPAT endothelial testing in 25
patients and found no correlation. I thus do not argue against beet root
supplementation but Beet Root alone is not the best approach.
Endothelial function is discussed in many of the audio-visual presentations
available for your review on heartfixer.com. I understand that all of this is
rather technical, but I want you to understand the factors that cause and
resolve cardiovascular disease. “Do as I say” medicine rather than “please
understand your disease process” medicine is also available to you, but this
will be a medicine confined to drugs and surgery. We will use drugs to improve
endothelial function and invasive therapies when appropriate (I’ve done over
5,000 invasive procedures and refer patients for bypass surgery and stent
placement when needed) but for my patients (and myself) I want something beyond
this. I want an integrative approach to cardiovascular and overall health, and
that is what you can expect from us.
James C. Roberts MD FACC FAARFM 12/23/23
* The herpes virus grows more rapidly in a high Arginine environment and is inhibited by lysine. If cold sores or other herpes virus related conditions develop in relation to arginine supplementation, add lysine 500 mg twice a day to your program.
** We can assess your nutritional status and level of oxidative stress with the Genova Labs NutrEval study, which is covered under Medicare (typical co-pay is $170 for private insurance).
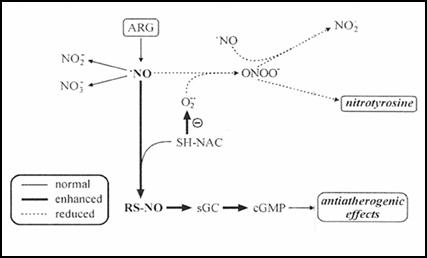
High levels of glutathione and cysteine within the endothelium help to maintain
a “ready reserve” of NO. N-Acetyl cysteine, lipoic acid, and glycine help
support the endothelial glutathione pool.
Free radicals such as superoxide degrade NO into peroxynitrite, a particularly
damaging free radical. Vitamin C squelches SO and methyl-folate neutralizes
peroxynitrite.

Angiotensin Converting Enzyme (ACE) not only generates Angiotensin II, but also degrades Bradykinin. Bradykinin up regulates the production of NO and Prostacyclin (PGI2 in the diagram), the metabolite of fish oil that protects against CV disease. Blockade of ACE within the endothelial cell preserves the vascular benefits of bradykinin.
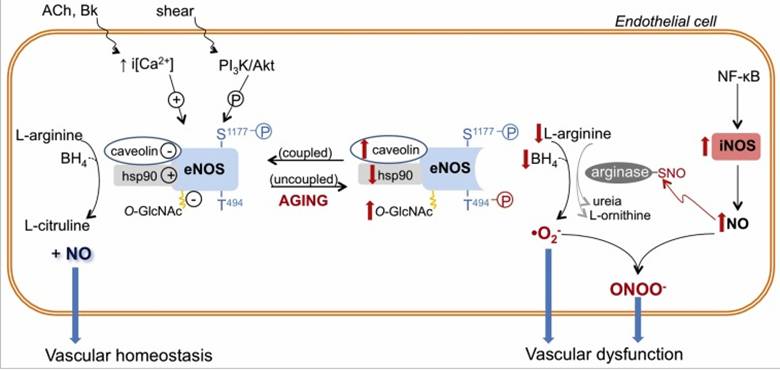
Phosphorylation of serine at the 1177th amino acid position within the NOS molecule, rapidly upregulates its ability to generate NO. Testosterone, estradiol, and DHEA increase the formation of NOS, but also activate the enzyme systems that phosphorylate serine 1177. This explains why intracoronary testosterone dilated coronary arteries and how IV or topical testosterone rapidly improves treadmill time in coronary patients.
Inflammation leads to up regulation in iNOS
(inflammatory NOS) which generates too much NO, at the wrong place and at the
wrong time. This activates the enzyme arginase, which degrades arginine,
increasing the ADMA:Arginine ratio and compromising endothelial function.
Thus, we wish to support our immune defenses while at the same time protecting
against inappropriate chronic inflammation.